Hormone therapy
Hormone therapy
Hormone therapy
Hormone therapy aims to block the production or effects of hormones, such as testosterone and dihydrotestosterone (DHT), that are produced by the testicles. It is used to slow the growth of cancer or to relieve pain or other symptoms (palliative care).
The role of hormone therapy
Has your doctor recommended hormone therapy to treat your prostate cancer? This video is for you! When it comes to hormone therapy, it pays to know the facts. Let’s take a closer look.

Why and for whom
Hormones called androgens (which include testosterone and DHT) contribute to the growth of prostate cancer cells. Hormone therapy is used to fight prostate cancer. It works by preventing your body from secreting or using these hormones, which slows down the growth and spread of your cancer. Hormone therapy treats your whole body rather than just targeting your prostate.
Hormone therapy can be administered
- As the primary treatment for advanced or recurrent prostate cancer.
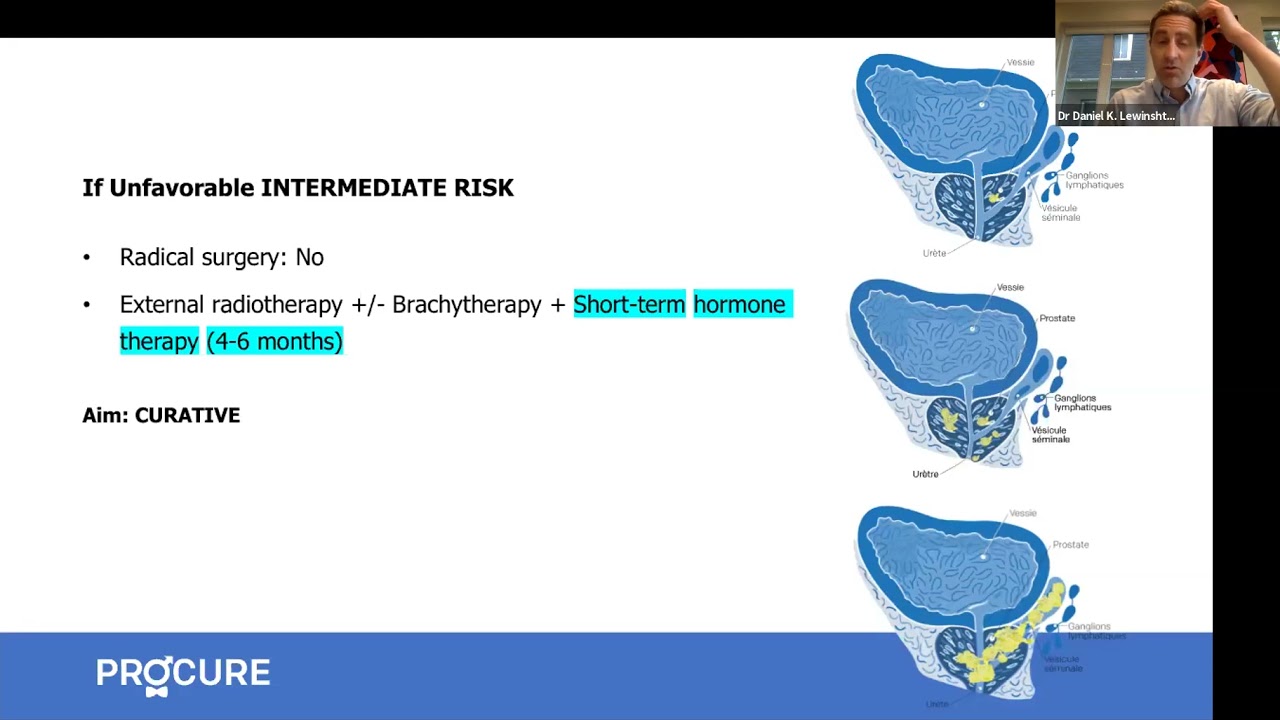
- Before, during, or after radiotherapy in cases of high-risk prostate cancer and in certain cases of intermediate-risk cancer.
- To relieve pain or manage symptoms of advanced prostate cancer (palliative treatment).
The most frequently used approaches and modalities
- Injectable medications that block testosterone production by the testicles.
- Oral medications that prevent prostate cancer cells from using testosterone or reduce the amount of testosterone that prostate cancer can use for growth.
- An intervention that involves removing the testicles, which produce the majority of testosterone in the body (to maintain appearance, artificial testicles may be inserted during the procedure).
Although these treatments can help relieve your symptoms, they do not lead to a cure. However, since they act on your whole body, they can help slow down the growth of your cancer, regardless of which parts of the body the cancer cells have spread to.
Is it for you
Hormone therapy aims to lower the amount of androgens (male hormones) circulating in your body and to slow down the growth of your prostate cancer. It achieves this by blocking testosterone production or blocking signals from your brain that instruct the testicles and adrenal glands (hormone secretors) to produce testosterone.
Male hormones are called androgens. Testosterone, the hormone responsible for the development of male sexual characteristics, is produced mainly by your testicles and to a lesser extent by your adrenal glands.
Testosterone stimulates the growth of your prostate. Cancer cells that can develop in your prostate are also stimulated by your testosterone to grow.
Hormone therapy is mainly used when initial treatments fail, including radical prostatectomy or radiotherapy.
Hormone therapy is also useful when a patient cannot undergo surgery or radiotherapy or refuses to undergo them. Occasionally, it may be combined with another treatment, such as radiotherapy.
Who can have hormone therapy?
- Men whose cancer has returned after another type of treatment (e.g., radiotherapy or surgery) or whose risk of cancer returning after these treatments is high.
- Men who do not qualify for surgery, radiotherapy, or brachytherapy.
- Men whose prostate cancer has spread outside the prostate and invaded other parts of the body (N1 or M1 stage).
- Men with very advanced cancer, as a way to control it and manage symptoms.
Neoadjuvant Hormone Therapy (before treatment)
Hormone therapy may be recommended a few months before your external radiotherapy or brachytherapy to shrink your tumor. This makes it easier to irradiate. This is called “neoadjuvant hormone therapy.” Hormone therapy before radical prostatectomy is not recommended.
Adjuvant Hormone Therapy (after treatment)
Adjuvant” hormone therapy is administered after radiotherapy or after radical prostatectomy. The doctor uses it when (due to your grade, stage, and PSA level) cancer cells may be spread throughout your body.
This does not mean you have metastases, but there is a risk of recurrence if isolated cells, often undetectable, remain in your body. The duration will be 4 to 6 months for an intermediate risk of recurrence and 2 to 3 years for a high risk of recurrence.
Concomitant Hormone Therapy (during treatment)
Concomitant” hormone therapy is administered during treatment, such as radiotherapy in cases of high-risk prostate cancer and in certain cases of intermediate-risk cancer.
Intermittent Hormone Therapy
Hormone therapy is stopped when PSA levels decrease and stabilize. It resumes when PSA levels start to rise again, which can take several months or even years. Intermittent treatment theoretically allows the patient to regain “normal” sexual activity and eliminate side effects during periods without medication.
It’s best to discuss this with your doctor.
Factors justifying this choice
Hormone therapy is considered to slow down the growth of prostate cancer but cannot cure it. When cancer is advanced, it is an excellent means of pain control.
However, the duration of its effectiveness varies among patients. From 70 to 85% of men who receive it respond to treatment for some time. For some, the respite can last more than 10 years, while for others, it will last less than a year.
Questions to my doctor
We invite you to consult our page Questions to ask to your doctor and your healthcare team regarding tests and diagnostic exams for prostate cancer. Asking questions will open up communication, provide information tailored to your situation, and reduce the stress associated with understanding the diagnosis of prostate cancer.
 To treat prostate cancer, hormone therapy offers numerous possibilities. Different molecules or combinations exist. While all act in the same way (chemical castration), they do not have the same side effects.
To treat prostate cancer, hormone therapy offers numerous possibilities. Different molecules or combinations exist. While all act in the same way (chemical castration), they do not have the same side effects.
The three main types
There are three main types of hormone therapy for prostate cancer.
- Injections or implants to stop your testosterone production
- Tablets to block the effects of testosterone
- Surgery, called orchidectomy, to remove your testicles
The most frequently used types of hormone therapy in the treatment of prostate cancer are:
- Luteinizing hormone-releasing hormone (LH-RH) analogs
- Luteinizing hormone-releasing hormone (LH-RH) antagonists
- Anti-androgens
- Estrogens
- Surgical removal of the testicles (orchidectomy)
LH-RH Analogues (or antagonists)
For hormone therapy before or after your treatment, the doctor mainly administers LH-RH analogs (or antagonists).
These medications prevent your testicles from producing testosterone (which feeds prostate cancer). By stopping testosterone production, the size of your tumor and prostate is reduced.
How it’s administered
The medication is administered by regular injections. Depending on the medication, the injection may be given every month or every 3, 4, or 6 months. Depending on the situation, this treatment may be given continuously for the rest of your life or intermittently depending on your cancer’s response.
The most commonly used LH-RH analogs are:
- leuprolide (Lupron, Lupron Depot, Eligard)
- goserelin (Zoladex)
- buserelin (Suprefact)
- triptorelin (Trelstar)
The LH-RH antagonist is:
- degarelix (Firmagon)
Anti-androgens
Anti-androgens work by blocking the effects of testosterone on your prostate cancer cells. The medication binds to androgen receptors on your prostate cancer cells, preventing them from using the testosterone present in your bloodstream.
You may be given anti-androgens for a short period if you are taking LH-RH analogs to alleviate a tumor flare reaction caused by the analogs.
How it’s administered
Anti-androgens can be taken orally in tablet or liquid form.
- As monotherapy
- Before receiving injections or implants
- Simultaneously with injections or implants
- After surgery to remove the testicles (orchidectomy).
The most common types are:
- bicalutamide (Casodex)
- flutamide (Euflex)
- cyproterone acetate (Androcur)
- nilutamide (Anandron)
Estrogens
Estrogens are female hormones that lower androgen levels. They are no longer used due to the cardiovascular problems they caused.
Orchidectomy
Orchidectomy is a form of hormone therapy that involves removing the testicles. It is a radical treatment since testosterone concentration can decrease by 90 to 95%. This procedure is also known as “surgical castration.” It is performed under regional anesthesia as a day surgery.
The advantage of orchidectomy is that the treated man does not need frequent injections of medication. The disadvantage of orchidectomy is that most men are sometimes afraid that this procedure will diminish their masculinity.
Advantages of hormone therapy
- It is an effective treatment for prostate cancer.
- It can treat prostate cancer no matter where it is in your body.
- It can be used with other treatments to make them more effective.
- It can help reduce some of the symptoms of advanced prostate cancer, such as urinary symptoms and pain related to metastases.
Disadvantages of hormone therapy
- It can cause side effects that could have a significant impact on your daily life.
- Some side effects, such as breast enlargement, are permanent.
- Used alone, hormone therapy does not cure cancer, but it can keep it under control, sometimes for several years.
- Its effectiveness may be of variable limited duration depending on the patients.
Risks and complications of hormone therapy
Medication-based hormone therapy has revolutionized the management of hormone-dependent cancers. However, the treatment, which can last for several years, often leads to side effects requiring appropriate management and support.
- Side effects can occur at any time during your hormone therapy. Some occur during treatment, others immediately after or a few days and even a few weeks later.
- Most disappear once hormone therapy is completed. Late effects may occur months or even years after treatment. Some side effects can last a long time or be permanent depending on the duration of your treatment.
- It is important to report any side effects to your doctor. They can assess (measure) the severity of some of them. Sometimes it may be necessary to adjust the dose administered if the side effects are significant.
Short – Medium term
Possible side effects, common to different types of hormone therapy, include:
- Decreased libido
- Erectile dysfunction
- Hot flashes
- Weight gain and loss of muscle mass
- Swelling and tenderness of the breasts (gynecomastia)
- Fatigue
- Irritability
Long term
Long-term use (more than one year) may lead to the following effects:
- Anemia
- Decreased bone mass (osteoporosis)
- Changes in masculine characteristics (e.g., testicular size decrease)
- Possible increase in the risk of cognitive (concentration, memory) or mood (depression) disorders
- Increased risk of cardiovascular diseases (heart attack, stroke, etc.)
- Increased risk of developing metabolic syndrome (diabetes, dyslipidemia, obesity, hypertension, etc.)
Results
Hormone therapy does not cure prostate cancer, but it is controlled. Therefore, you can live longer and maintain a good quality of life. This varies depending on each case because it is necessary to consider the diagnosed grade of the tumor, its stage of spread, and the PSA level before treatment.
The dosage of prostate-specific antigen (PSA), performed regularly – every three to six months – and occasionally, the digital rectal exam, allow your doctor to monitor your condition. The lower the level drops, the better the chances that the cancer is controlled.
However, the goal is not so much to achieve a PSA level of 0 ng/mL as it is to stabilize this level (if you have also undergone radical prostatectomy, the PSA should be undetectable). As long as it remains stable, everything is fine.
Recurrence
At each consultation, a blood test allows your doctor to monitor your PSA level. If the PSA level starts to rise, the doctor will monitor how long it takes to double. The shorter this period, the higher the risks of recurrence and the more aggressive the recurrence will be. Prostate cancer will then have become castration-resistant cancer (formerly known as hormone-refractory). If this is the case, other treatments should be considered.
The following article “You are no longer responding to hormone therapy and have no metastases?” will give you some guidance on what to do next.
Hope and Advances in Research
Testimony of Robert and his son Jean-Marc Evenat
To see our other testimonies, click here.
Side effects
Regardless of the treatment for prostate cancer, it is always possible for some side effects to occur. However, they do not affect everyone; if they do, not everyone experiences them in the same way. The side effects of hormone therapy depend mainly on the following factors:
- Your type of hormone therapy (surgery or medication)
- The type of medication used and the duration of treatment
- Your overall health
These adverse effects, although transient, can be difficult to manage, and some patients may be tempted to stop treatment. However, it is important to keep in mind the major therapeutic impact of hormone therapy. Moreover, there are usually ways to relieve these symptoms and help the patient overcome them. To learn more, consult our section on side effects related to hormone therapy
Do not hesitate to discuss all your side effects with your doctor during your follow-up visits.
Additional Information - Treatment options
Advanced prostate cancer treatments strategies
Strategies for treating advanced cancer have significantly evolved, offering new options and hope for patients.
Prostate Cancer Study Results Summaries (2023 ASCO-GU)
Summary of clinical trial results on promising prostate cancer research.
Advanced Prostate Cancer Triple Therapy Study Results (2023 ASCO-GU)
Clinical trial results on triple therapy for advanced hormone-sensitive prostate cancer.
Expert Opinion: Prostate Cancer and Hormone Therapy
What you need to know about hormone therapy and how to manage the side effects of this treatment.
Prostate cancer and nuclear medicine
What about nuclear medicine? Is it suitable for your situation?
Nuclear imaging technologies
Has your doctor suggested prostate imaging tests? Explore options like PSMA PET scans.
Targeted therapy and inherited mutations
If you have a specific genetic mutation, you could benefit from new targeted treatments.
States of prostate cancer following treatment
Do your recent tests show an increase in PSA levels? It could indicate a recurrence.
The role of hormone therapy
Has your doctor recommended hormone therapy? This video is for you!
Advanced prostate cancer treatment strategies
Strategies for treating advanced cancer have significantly evolved, offering new options and hope for patients.
Advanced prostate cancer treatment
Advanced prostate cancer encompasses various conditions, including metastatic, recurrent, and hormone-resistant forms, each raising different questions and concerns.
When prostate cancer comes back
A recurrence is when the cancer returns after treatment. The main question is, “What’s next?”
How to treat advanced prostate cancer
Advanced prostate cancer encompasses various conditions, including metastatic, recurrent, and hormone-resistant forms, each raising different questions and concerns.
All about hormone therapy
Hormone therapy can reduce tumor size, control cancer, and prolong life. Is it the right treatment for your cancer?
Q-A – New therapies for advance prostate cancer
In this interview, we answer patients’ questions about new therapies for advanced prostate cancer.

Do your medications cause erectile dysfunction?
Aside from prostate cancer treatments, if you experience erection problems such as erectile dysfunction, it’s crucial to understand that this can be related to various causes. Often, erectile dysfunction is triggered by reduced blood flow to the penis or issues affecting the nerves responsible for erection. These situations frequently arise from other health problems such […]

Vacuum erection devices: What you need to know
Vacuum erection devices (VEDs), or penile pumps, are a non-invasive solution for men experiencing erectile dysfunction (ED), particularly after radical surgery to treat prostate cancer. These devices can help restore erectile function, improving quality of life and intimacy. Let’s explore what to look for when buying a VED, the benefits of choosing a medical-grade device, […]

Living with permanent erectile dysfunction in 5 points
Living with permanent erectile dysfunction in 5 points outlines the essential considerations in navigating this reality. These tips serve as guiding principles to assist individuals, whether they are in a relationship or facing this situation alone. Healthcare professionals are here for you Sexuality is ever-present; it does not disappear with permanent erectile dysfunction. Consult healthcare […]

Sexuality and intimacy in 5 points
Sexuality and intimacy in 5 points addresses specific challenges and opportunities that may arise after treatment for prostate cancer.

Orgasm without erection?
It is entirely possible for a man to achieve orgasm without an erection or penetration and there are several ways to achieve this.

Food tastes funny…!
I feel like one of the worst effects was losing my taste buds. Everything I tried to eat tasted funny. So why food tastes funny?

I am a little bit diabetic
My doctor informed me that I am a little bit diabetic and that I will have to make important changes to my lifestyle.

Will the effects of hormone therapy disappear?
Hormone therapy is used to prevent your body from secreting or using testosterone. But what about the side effects of hormone therapy?

Why am I urinating my semen
If you are wondering why you urinate your semen, the answer is that you have what is called retrograde ejaculation.
Sources and references
Last medical and editorial review: April 2024. See our web page validation committee and our collaborators by clicking here.


