Brachytherapy
Overview
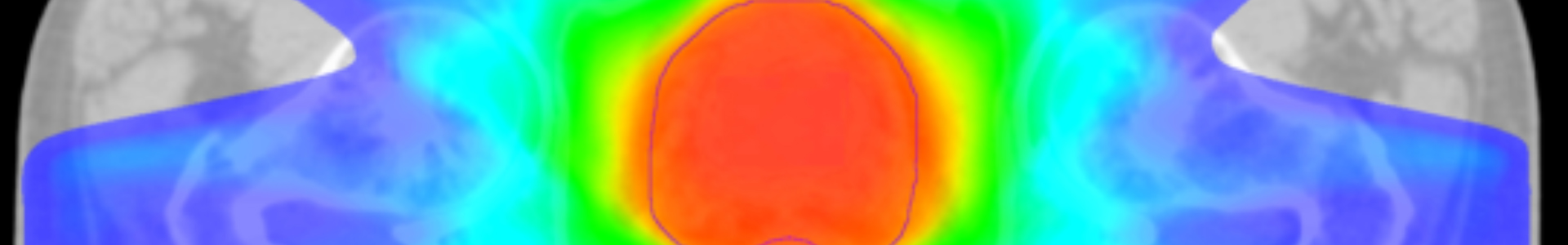
 The word brachy- originates from the Greek word brachys, meaning “short”. Therefore, “brachytherapy” means treatment with radiation therapy at a short distance, as opposed to “teletherapy”, also known as external beam radiotherapy. Brachytherapy is a type of radiation therapy involving the insertion of radioactive materials directly in the specific tissue being treated, in this case, the cancerous prostate. The major advantage of brachytherapy is the delivery of a high dose of radiation to the diseased organ while sparing the surrounding normal organs.
The word brachy- originates from the Greek word brachys, meaning “short”. Therefore, “brachytherapy” means treatment with radiation therapy at a short distance, as opposed to “teletherapy”, also known as external beam radiotherapy. Brachytherapy is a type of radiation therapy involving the insertion of radioactive materials directly in the specific tissue being treated, in this case, the cancerous prostate. The major advantage of brachytherapy is the delivery of a high dose of radiation to the diseased organ while sparing the surrounding normal organs.
Types of brachytherapy
Brachytherapy is administered in two ways:
- Low dose rate brachytherapy: the radiation dose for this treatment is very low but permanent. Permanent implants, like radioactive seeds, are not removed. They release radiation over several weeks or months.
- High dose rate brachytherapy: a source of high dose rate radiation is inserted into the prostate gland. Temporary implants are removed once the desired dose of radiation is delivered.
Brachytherapy is usually used to treat low- and intermediate-risk prostate cancer. Combined external beam radiation therapy and brachytherapy may be used for cases of high-risk prostate cancer.
Radioactive materials most frequently used in brachytherapy to treat prostate cancer are Iodine, Iridium, and Cesium.
The time it takes for half of a material’s radioactivity to disappear is called the half-life. Different radioactive materials have different half-lives. This information helps the radiation therapy team choose the type of material to use and plant the treatment regimen. It also determines how long radiation safety precautions must be taken following treatment.
Is it for you
Permanent or Low Dose Rate Brachytherapy

Low dose rate brachytherapy, often called by its acronym LDR (Low Dose Rate), uses very low levels of radiation. Radiation is emitted from small radioactive sources containing radioiodide Iodine-125.
These sources look like grains of rice and are permanently implanted into the prostate. The radiation gets weaker with time and after 6 months 95% of the radioactive material is used up. Permanent implants do not cause any long‑term problems.
This form of treatment is recommended for patients who have been diagnosed with a localized prostate cancer that is still relatively early stage (T1, T2a), growing slowly and thus at a low risk of progression (Gleason 6 or less) and low PSA rate. Brachytherapy may be an option for cancers of intermediate risk of progression (Gleason 7), but patients are selected according to a highly specific criteria.
Temporary or High Dose Rate Brachytherapy

HDR stands for “high dose rate”, the term that describes the delivery of high doses of radiotherapy within a short time interval. They are released from small sources containing radioactive iridium, called “iridium 192”.
This type of brachytherapy could be administered either as a boost (extra dose of radiation to the prostate alone) to external beam radiation therapy, or as sole treatment for prostate cancer (known as HDR mono therapy), with ur without hormone therapy.
Used as a boost: HDR brachytherapy is increasingly being considered as a means of dose intensification in any patient receiving external beam therapy for the treatment of prostate cancer. It thus reduces the number of treatments of conventional radiotherapy. This approach is particularly useful for patients with intermediate and high risk of disease progression.
Used in monotherapy: Although not recommended as a single treatment for patients with prostate cancer at high risk of progression, monotherapy for low-risk or intermediate-risk of prostate cancer progression is a common treatment used today
Additional considerations
Brachytherapy can not be recommended:
- To men who have symptoms of prostatitis linked to a urinary obstruction or who have undergone transurethral resection of the prostate (TURP).
- To men whose prostate cancer has metastasized, according to bone scans or CT scans of the abdomen and pelvis.
- To men who have undergone pelvic radiotherapy, who have hip problems or who are subject to any other contraindication.
Note
- Because this competency and technology are expensive, this treatment is not available in all hospitals across Quebec.
Reasons for choosing HDR brachytherapy
For many men with localized prostate cancer, brachytherapy offers an effective treatment without the risks and recovery time that come with surgery.
Advantages and limitations
 Advantages of brachytherapy
Advantages of brachytherapy
- Recovery is quick. Most men can return to their normal activities soon after treatment.
- No hospitalization is required as it is a one day procedure.
- Radiation does not travel through the skin or into other healthy organs to get to cancer cells. Brachytherapy causes less secondary damage to neighbouring organs.
- Less demanding of a treatment than traditional radiation therapy and less taxing than radical prostatectomies.
- There is no recovery period or operative stress as with a radical prostatectomy.
Limitations of brachytherapy
- Late onset side effects can affect bowel and erectile functions, including reduction of ejaculate and infertility.
- You will usually need to have a general anaesthetic—which can have side effects.
- Unsuccessful procedures cannot be treated surgically—eliminating an important treatment option.
- It may be some time before you know whether the treatment has been successful.
- You will need to avoid sitting very close to pregnant women or children for more than a few minutes each day, for the first three months after treatment.
Risks and complications of brachytherapy
Some side effects occur immediately after your treatment or a few weeks later. In general, they are temporary, can last a few months and gradually disappear in the year following the end of treatment.
Short-Medium term
The side effects of brachytherapy are similar to those of external radiotherapy, but differ slightly. Piercing the prostate several times causes it to swell. This can cause urinary problems, the symptoms of which can manifest by:
- frequent urges to urinate, especially at night
- urge to urinate (urgency)
- difficulty urinating with a weaker jet
- burning sensations during urination, sometimes even complete blockage of urine (acute retention of urine)
Pain in the perineum, blood in the urine or sperm, transient erection problems may occur following treatment.
Irritation of the bowels and rectal disorders, such as inflammation of the rectum, are uncommon. On the other hand, though very rare, diarrhea, anal irritation, or rectal bleeding may occur in the months following treatment.
Side effects may be greater if brachytherapy is high dose and complementary to external beam radiotherapy.
Long Term
Long-term effects can appear months or years after treatment. Side effects vary but can include:
- Erectile dysfunction
- Significant decrease in ejaculate and infertility
- Risk of urinary incontinence or symptoms of chronic urinary obstruction are rare (less than 5% in both cases).
Side effects do not affect all men in the same way. They depend greatly on your state of health before treatment. It is important to report any side effects to your doctor. Whether short-, medium-, or long-term, most can be relieved by taking medication or through other interventions/methods.
What to expect
 Your doctor has offered you a brachytherapy treatment to treat your prostate cancer? This section describes this treatment and the precautions to be taken to ensure that everything goes as smoothly as possible.
Your doctor has offered you a brachytherapy treatment to treat your prostate cancer? This section describes this treatment and the precautions to be taken to ensure that everything goes as smoothly as possible.
Terminology
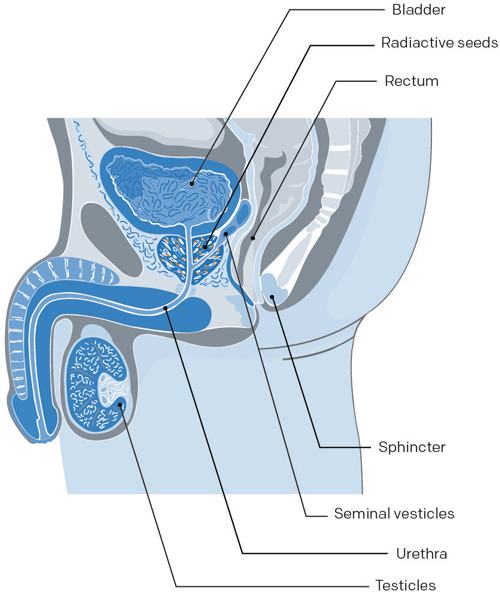
To familiarize you with medical language, here is a brief description of structures that make up the male reproductive system.
Bladder: The muscular sac-like organ in which urine is collected and stored in the body.
Prostate: The gland located just below the bladder that surrounds the urethra. It secretes fluids that mix with sperm cells to form semen.
Rectum: The terminal section of the large intestine.
Sphincter: Small muscles located at the opening between the bladder and the prostate. The sphincter prevents urine from leaking out of the bladder—controlling urinary continence.
Seminal vesicles: Small pouches alongside the prostate that store sperm produced the prostate.
Urethra: The tube that carries urine from the bladder and sperm secreted by the genital glands out through the penis.
Testicles: The two glands located inside the scrotum that form sperm cells and produce testosterone (male hormone).
Modalities for brachytherapy (LDR)
Duration of the intervention
The procedure takes 1–2 hours. However, including the preparation, calculations, and recovery, the procedure may take up to 8 hours.
Installation of a urinary catheter
A spinal anesthesia is administered locally—in rare cases, a general anesthesia is used. During the procedure, a urinary catheter is set in place during the procedure and is taken out at the end. In very rare cases, the catheter may be left in place to help you urinate for a variable period of time.
The intervention
A transrectal ultrasound will be used to accurately place the pellets throughout the prostate in the pre-planned positions. An experienced radiation oncologist will place between 80 and 100 radioactive pellets in the prostate.
Grain identification
The radioactive pellets implanted in the prostate will gradually kill your cancer cells in the following hours and days. A special CT scan will be performed 3–6 weeks after the procedure for the final seed position assessment and dose calculations.
Your PSA level
With LDR brachytherapy, PSA levels will generally not fall all the way down to 0 ng/mL because it is almost impossible to destroy 100% of prostate cells. In general, the PSA level will drop and then stabilize.
Modalities for brachytherapy (HDR)
Duration of the intervention
The procedure takes two to three hours in the treatment room and the patient can leave in the evening. In rare cases, the doctor may decide to keep him longer.
Installation of a urinary catheter
A general anesthesia is administered. During the procedure, a urinary catheter is set in place during the procedure and is taken out at the end. In very rare cases, the catheter may be left in place to help you urinate for a variable period of time.
The intervention
The doctor will introduce plastic tubes (from 12 to 18 or even more catheters) into the skin, between the scrotum and the anus. The tubes are then inserted through the body cavities to the prostate with the aid of a probe. The tubes are connected to a treatment device that sends a radioactive source (Iridium 192) through the tubes. The treatment lasts between 20 and 30 minutes.
Your PSA level
With HDR brachytherapy, PSA levels will generally not fall all the way down to 0 ng/mL because it is almost impossible to destroy 100% of prostate cells. In general, the PSA level will drop and then stabilize.
In monotherapy
In cases of HDR monotherapy, the treatment consists of one to two doses in a same-day surgery setting. For the duration of the treatment, the patient remains in hospital. Since there is no radioactivity when the catheters are not connected to a machine, the patient rests in the general urology unit, with no need for isolation.
Getting ready
 Being well-prepared will help you recover more quickly and be less stressed. By reading the following, you will know exactly what is waiting for you.
Being well-prepared will help you recover more quickly and be less stressed. By reading the following, you will know exactly what is waiting for you.
Before your brachytherapy
Be active
It is important to move to stay healthy, even if you have prostate cancer. Consequently, if you’re already practicing a regular activity, you should continue doing it. If this is not the case, it’s never too late to add exercise to your daily routine; even if it’s at a lower intensity.
Even taking a short 15–30 minute walk can be beneficial.
Try to stop smoking
Even if it’s stressful, it is recommended that you stop smoking 6 weeks before your surgery in order to reduce the risks of lung, healing, and infection problems. If needed, your doctor may prescribe medication to help you.
Reduce your alcohol consumption
Alcohol can also interact with medication. This is why it is recommended to reduce its consumption and not drink in the 24 hours before surgery.
Adopt good eating habits
A healthy and balanced diet will also help you to recover quickly after your treatment. Energy, proteins, vitamins, and minerals that you get from your food can help fight against these infections and help contribute to your healing.
Basic advice for you
- Have 3 meals a day and snacks when you need them.
- Eat food from all four of Canada’s Food Guide (low-fat dairy products, fruits and vegetables, grain products, lean meat, skinless poultry, fish, and other alternatives) in order to ensure you get your daily intake of various nutrients.
- Have at least one meal a day that consists of lean meat, skinless poultry, or fish in order to ensure you get your daily intake of various nutrients.
- Fruits and vegetables are an excellent and important source of vitamins and minerals.
- Drink enough water—at least 1 500 mL a day or 6–8 glasses.
Your medication
Ask your doctor what to do before you stop taking your medication.
Avoid natural products
If needed, discuss it with your doctor first.
Arrange transportation
You should be able to leave the hospital the same day if everything goes smoothly. You will not be able to drive home. Thus it is recommended that you have someone accompany you when you leave.
Before starting your treatment
Shortly before starting your treatment, you will meet with your medical team in order to prepare you for it.
A few weeks before your treatment
You may receive a call for a preadmission appointment. You will undergo various tests to complete your checkup.
One week ahead of your high dose brachytherapy treatment, start taking the medication that your doctor has prescribed to help you urinate.
The night before your treatment
You should not drink or eat anything after midnight. If you need to take medication, you can have a little bit of water. You will have to give yourself a rectal enema at home, as explained to you.
The day of your treatment
Inform the doctor of all medication you usually take. Bring them in their original containers. You will be given an antibiotic intravenously before the operation.
Bring comfortable loose-fitting underwear and absorbent protection to the hospital. You will be more comfortable when you return home.
During treatment
 During your brachytherapy (LDR)
During your brachytherapy (LDR)
Your medical team will tell you exactly what treatment is planned for you. Do not hesitate to ask them all your questions.
- Antibiotics will be given intravenously before the procedure.
- The procedure lasts 1–1.5 hours.
- The procedure is performed under local anaesthesia. The lower half of your body is “frozen”, but you are not asleep. Some patients however are put under. Once anesthetized, a catheter is put in place.
- An ultrasound probe is used to better see the prostate and to correctly implant radioactive pellets. This small tube, inserted through the rectum, provides clear images of the prostate, urethra, and rectum and then stores these images in the computer. The goal is to optimize irradiation, so as to best treat the tumor while avoiding the surrounding healthy organs.
- The ultrasound enables the pellets to be inserted into the prostate with a needle. The needles are inserted through the perineum (the area between the testicles and anus). The pellets (between 40 and 60) are placed with extreme precision.
- No cuts are made. When the needles are removed, just as with a blood test, the skin closes immediately.
- At the end of the procedure, you are brought to the recovery room.
- Usually, the urinary catheter is removed before you leave the hospital. Otherwise, this is usually done the next day in a CLSC. Normally, you leave the hospital that evening.
During your brachytherapy (HDR)
Your medical team will tell you exactly what treatment is planned for you. Do not hesitate to ask them all your questions.
- The procedure takes about 2 hours.
- The procedure is performed by an experienced radiation oncologist, in conjunction with a urologist.
- This treatment is done while you are “asleep” (general anesthesia or given as an epidural). So you do not feel pain during the treatment and you do not move, which is very important. A sedative may be offered before anesthesia.
- A urinary catheter is installed. It is a tube that enters through the penis and that allows you to urinate.
- The doctor will introduce plastic tubes (from 12 to 18 or even more catheters) into the skin, between the scrotum and the anus. The tubes are then inserted through the body cavities to the prostate with the aid of a probe. At this stage, no radioactive source is added. The procedure lasts about 45 minutes.
- The medical team will ensure that the tubes are properly in place. Depending on the center, the simulation is done by ultrasound or scanner after implantation. They will perform a computer simulation to ensure the complete treatment of the prostate and all targeted tissues. The main advantage of this kind of simulation is that it allows for the optimization of doses. This method aims to ensure the homogeneous treatment of the prostate is administered and that the effects on the normal structures (like the urethra, the rectum and the bladder) are reduced.
- The tubes are connected to a treatment device that sends a radioactive source (Iridium 192) through the tubes. The treatment lasts 20 to 30 minutes.
- Then the tubes are removed and you will be taken to the recovery room.
- Generally, the urinary catheter will be removed before you leave the hospital. Otherwise, it will be done the following day.
Your return home and instructions to follow are similar to those described for external radiation therapy.
At home
 Your recovery
Your recovery
HDR brachytherapy: Your return home and instructions to follow are similar to those described for external radiation therapy.
Low dose brachytherapy has a short recovery period.
You will be able to resume normal activities and some sports within a few days of your procedure. However, at home, do not exert yourself. Avoid heavy physical exertion for at least 4 weeks.
- No cycling
- No gym training
- No moving
Will I experience discomfort after treatment?
You may experience on or more of the following side effects:
- Bruising may appear on the testicles or penis immediately after treatment or several days later. This is normal and usually not very painful. To relieve bruising, apply ice to the affected area and take pain killers.
- Blood can be found in your urine a few hours or a few days after your treatment. This is normal. If you see small clots or lumps of blood in your urine, drink a lot of water and it should pass.
- In the month following your treatment, you may need to urinate more often. You may also feel a slight burning sensation when urinating. If this is the case, speak with your doctor—medication can help.
- Bowel movements may cause some pain if your anus is irritated. Some people will also have diarrhea. These rare side effects go away about 5 weeks after treatment, but can occasionally recur.
Important
If you are unable to urinate, call your radiation oncology clinic. Outside business hours, call 9-1-1 to get emergency medical help or go to the hospital emergency department.
When will I see my doctor?
You will meet with your doctor 1 month after your treatment in order to ensure that radioactive pellets are staying in place and to control the dose you receive. He will take an x-ray of your prostate if you have received temporary brachytherapy (HDR). After, you will see your doctor—alternating with your urologist— every 3-4 months, for at least 5 years.
Who should I notify if I cannot make my appointment?
Call the radiation oncology department as soon as possible.
Who should I contact for help or to ask questions?
If you have any questions or concerns:
- During the day or week, call the radiation oncology department and ask to speak to your clinical counsellor.
- During the evening or weekend, call the hospital directly and ask to speak with the radiation oncologist on duty.
Sex and safety measures
Given that you are carrying radioactive sources, certain precautions need to be taken.
In the first three months after the procedure
- Pregnant women should maintain a distance of 1 metre (3 feet) from the patient.
- Children under twelve should not sit on the patient’s lap for an extended period of time (no more than 5 hours per day), but can sit next to them.
There is no indication that sleeping in the same bed as your spouse is dangerous, unless pregnant.
Transmission
Radioactive pellets do not make bodily fluids, such as urine or semen, radioactive. There is no danger of radiation transmission to a partner.
- Men who engage in sexual activities immediately after this procedure sometimes experience a burning sensation or pain during ejaculation.
- In addition, they may also notice blood in their semen. This symptom presents no danger to either the man or his partner and will go away with time.
Implant displacement
The risk of the radioactive pellets moving is minimal. Ejection of a seed during sexual intercourse is extremely rare.
- However, according to experts, even if a pellet is ejaculated into the partner it is not dangerous.
- To further ensure the protection of your partner, some doctors recommend the use of a condom for at least the first 5 ejaculations or every time if your partner is pregnant. After a while, the pellets become inactive and remain permanently in your body without causing any harm. Your doctor will give you more details after your procedure.
Medical follow-up
 The importance of follow-ups
The importance of follow-ups
Medical certificate
If you need a medical certificate, don’t forget to ask your radiation oncologist.
Results
As with radical surgery and radiation therapy, it is impossible to estimate the average success rate of brachytherapy.
- Success will vary from person to person because of individual differences in the grade of the tumour, the degree to which the cancer has spread, and the PSA level before treatment.
- The less severe these three factors are, the better the patient’s chances are of being in the clear.
PSA tests
Every 3-4 months, a digital rectal exam is performed and your prostate‑specific antigen (PSA) level is measured since this test is the best predictor for the risk of recurrence of prostate cancer.
Your PSA level
With brachytherapy, PSA levels will generally not fall all the way down to 0 ng/mL because there are still normal prostatic cells left. Your PSA levels should begin to drop in the months following the start of treatment and may continue to drop for as long as a year after treatment ends. In general, after dropping, it remains stable.
At each medical appointment, your urologist will check 3 parameters:
- if the PSA level is higher
- how much time has it been since the operation and
- how much time does it take this level to double (velocity)
Recurrence
If the PSA level starts to climb, the doctor will monitor how much time it takes to double. The shorter these periods are, the greater the risk of recurrence and the more aggressive the recurrence will be. For example, the PSA level that starts to increase eight months after the treatment and that doubles in four months is much more worrisome than a PSA level that starts to climb three years after the treatment and takes a year to double.
If necessary, hormone therapy may be prescribed.
Remission
You will be monitored for at least five years after your treatment. If everything goes well, after seven to ten years without recurrence, the risk of recurrence is very low.
Side effects
 The side effects of brachytherapy depend on the following factors:
The side effects of brachytherapy depend on the following factors:
- the type of implants (temporary or permanent)
- the volume of the area treated
- the irradiation dose reaching the neighboring organs (usually very low)
- the total dose received
Some side effects occur immediately after the procedure or a few weeks later. In general, they are temporary. Others appear well after the treatment and can last for a long time.
The most common problems associated with brachytherapy are urinary, gastro-intestinal, and erectile functional problems.
Intestinal and urinary functions
Sometimes intestinal and urinary functions do not return to normal after treatment is complete. This happens to 5–10% of men.
- Some medications (such as cortisone that reduces rectal inflammation) and muscle relaxants can sometimes help alleviate these symptoms.
- Make an appointment with a nutritionist or dietician for your intestinal problems.
- Discuss your urinary problems with your doctor. Urinary problems can often be easily corrected with medication or a procedure.
Erectile Function
Erectile problems
The percentage risk of erectile dysfunction varies for each patient. However, unlike other side effects, erectile dysfunction appears gradually several months or even years after treatment, but does not affect one’s enjoyment.
- As cellular death happens gradually, you will still be able to have an erection at first, but may slowly lose the ability with time.
- Your erectile capacity depends on your sexual function before treatment, your age, your general state of health, and the preservation of your erectile nerves during radiation therapy.
ED treatments
When you start experiencing erectile dysfunction, your doctor will prescribe medication that will help you regain your erectile capacity and a satisfying sex life.
Treatments include oral medication such as tadalafil, sildenafil, vardenafil; the MUSE pellet; penile injections; vacuum pumps; or surgical penile implants.
Your libido and orgasms
Your libido and ability to have orgasms remain intact. It should be stressed that your orgasm (feelings of enjoyment) is not affected since it is controlled by other nerves located far from your prostate.
Your ejaculations and loss of fertility
Brachytherapy irradiates your prostate, so you can expect a significant decrease in the ejaculate. Seminal liquid, that you will no longer produce, keeps your sperm cells healthy, which is why you usually become infertile.
If you want to have children, you will need to call a sperm bank. Discuss it with both your doctor and partner.
Suggestions and advice
 Give yourself time
Give yourself time
- There is a lot of information to retain. Don’t try to learn it all in one day.
- You will have questions. Write them down and bring them with you to your next appointment.
- Your body needs time to recover during treatment.
A healthy lifestyle will help you feel better
- Eat healthy
- Sleep a lot
- Do activities that you enjoy and that relax you
- Socialize
Accept help from others, they want what is best for you
- Practical help
- Emotional support
- Delegate tasks if you need to
- Do not be embarrassed to ask for help
Spend time with others and give them your attention
- Your friends and family also need comfort
- Keep a good line of communication open
- Resolve problems when they happen
Questions to my doctor
Here is a list of questions about brachytherapy for you to ask your doctor and healthcare team.
Read more…
- What type of brachytherapy is used for this cancer?
- When will brachytherapy begin? Is there a waiting list?
- Where will brachytherapy be administered?
- Is it necessary to be hospitalized for brachytherapy? If so, for how long?
- Is it possible to be accompanied by a caregiver (spouse, relative or friend for example) during the brachytherapy?
- What are the chances of treatment being effective? When will we know?
- Is preparation necessary before brachytherapy?
- What tests are done during brachytherapy?
- Will other treatments be given at the same time?
- Can vitamins or over-the-counter medications (e.g. Tylenol) interfere with brachytherapy?
- What are the possible side effects of brachytherapy? When could they appear? In general, how long do they last?
- What side effects should I report immediately? Who should I call?
- What can be done to relieve side effects?
- Will a special diet be required?
- Are there special things to do or not to do during and after brachytherapy?
- Will brachytherapy affect my usual activities? If so, for how long?
- Will other treatments be required after brachytherapy? If so, If so, what kind?
- How often are follow-up visits scheduled? Who is responsible for follow-up after brachytherapy?
- Are there special instructions for travel? At airports?
We are here for you
You have questions or concerns? Don’t hesitate. Contact us at 1-855-899-2873 to discuss with one of our nurses specialized in uro-oncology. They are there to listen, support and answer your questions, and those of your family or your loved ones. It’s simple and free, like all of our other services.
Also take the time to visit each of our pages on this website, as well as our YouTube channel, in order to get familiar with the disease, our expert lectures, our section on available resources, the support that is offered to you, our events and ways to get involved to advance the cause.
Staying Informed
Pages that might interest you
Want to know more? Just click on one of the links below.
The latest PROCURE news that might interest you
Every week we publish a blog article. Here are some we have chosen for you.
- Did you say prostate cancer?
- I want to postpone my treatment… Is that wise?
- I have several treatment options… Which one to choose?
The medical content and editorial team at PROCURE
Our team is composed of urologists, and nurses certified in uro-oncology with a deep knowledge of prostate cancer and other diseases related to the genitourinary system. Meet our staff by clicking here.
Sources and references
- Prostate Cancer – Understand the disease and its treatments; Fred Saad, MD, FRCSC and Michael McCormack, MD, FRCSC, 4th et 5th editions
- Canadian Cancer Society
- Prostate Cancer Foundation-PCF.org
- National Cancer Institute-USA
- American Cancer Society
- Memorial Sloan Kettering Cancer Center
- Prostate Cancer UK
Last medical and editorial review: September 2023
Written by PROCURE. © All rights reserved



