Depression and anxiety
- Side effects
- Depression and anxiety
- Recognizing changes in your m...
- Useful tips
- Who can help

Depression and anxiety
The diagnosis of prostate cancer, its treatment, the side effects thereof, or even the side effects related to hormone therapy, chemotherapy, or other oral treatments for advanced cancer, are stressful and life-changing events. It is normal to feel lost, anxious, nervous, sad, depressed, or depressive.
Overview
Some symptoms of anxiety and stress include:
- Excessive worrying, or restlessness
- Trouble sleeping, tiredness and exhaustion, or excessive sleeping
- Muscle tension
- Fast heartbeat, trembling, chest tightness, high blood pressure, nausea, dizziness, and shortness of breath
- Trouble concentrating, irritability, or impatience
Some symptoms of depression, especially in older people, include:
- Feelings of sadness, emptiness, hopelessness, anger, and irritability or frustration
- Problems with memory, concentration, confusion, or personality changes
- Sleep problems
- Losing interest in going out and socializing
- Loss of self-esteem
- Isolation
- Suicidal thinking
If you find that your symptoms last for most of the day, every day, for more than two weeks, you should speak with your doctor and get help.
What causes anxiety and depression?
It is important to understand that it isn’t a sign of weakness or failure, or your inability to cope with your diagnosis. Anxiety and depression can be different for everyone.
About 40–45% of men require psychosocial counselling at some point during their treatment for one reason or another.
- Fear of recurrence
- Long-term side effects of treatments
- Anxiety and dealing with recurrence
- Anxiety and accepting death
- Depression
Psychological counselling should be an integral part of your treatment
- To prevent and treat the impact of the disease on the patient and their loved ones
- To find ways to help you get through this difficult time
For more information take a look at our Coping with cancer and I have advanced cancer sections.
Tips for managing your mood
Knowledge is power
Some people feel less anxious knowing everything about their cancer treatment, while others get stressed out with all the details. Figure out where you feel the most comfortable to help control treatment‑related anxiety.
Identify your triggers
Use a journal to write down your feelings and help you identify the events that make you feel the most anxious or depressed—then you can figure out how to deal with them. Don’t forget to record good things too!
Talk it out
Start by talking with just one person about your feelings—it could be a family member, friend, or someone who’s lived through a similar cancer experience. All it takes is one conversation to open up and start feeling better. Visit our Support for you section and call 1 855 899‑2873 to speak to one of our uro‑oncology specialists.
Surround yourself with positivity
Whether it’s people, events, or pets, surround yourself with things that make you happy and do things that you enjoy.
Eat well and stay active
A healthy diet helps maintain proper nutrition and exercise releases natural mood boosters called endorphins. Try low‑impact and stress‑relieving activities like yoga.
Cut down on caffeine
As part of a healthy diet, monitor the amount of caffeine (a stimulant) you consume in drinks like coffee, tea, or coke. You can easily start cutting back by switching to a decaf version of the same drink.
The first person who can give you psychological help is your urologist. He will be assisted by your radiation oncologist if you need or are undergoing radiation therapy and your hemato-oncologist if chemotherapy becomes necessary.
So when distress or difficulties arise, many hospital staff can help you. The choice of a health professional is primarily based on the nature of the problems, but also according to your preferences. In order to make an informed decision, it is important that you discuss this with your doctor (urologist, radiation oncologist, hemato-oncologist) or with any other member of the team who accompanies you in your medical follow-up. Do not neglect your family doctor, because he can, like your specialist, help you; he will take into consideration your overall state of health and will refer you, if necessary, to the right specialist.
You can take advantage of the contribution of several health professionals at the same time or successively during your medical journey. Visit the Resources section of our site for more information or contact us at 1-855-899-2873. Other health professionals for you:
The psychiatrist
The psychiatrist is a medical specialist who can diagnose psychosocial problems, evaluate underlying physical disorders, and prescribe medication. They can also treat patients for pain. A psychiatrist can help the patient both physically and psychologically.
The psychologist
The psychologist can help in coping with emotional or psychological reactions to the disease and its treatments. They can also help in understanding the reaction of family members. Psychiatrists can help improve your quality of life, psychological health, and the family’s coping abilities.
The sexologist
A sexologist can help the patient and his partner overcome or adapt to the changes in their sexuality that take place after treatment. For example, the sex therapist can help patients cope with erectile dysfunction naturally without medication. They can also help patients explore other sides of their sexuality and find different ways of expressing affection.
Sexuality can take on different forms yet still remain equally fulfilling for both spouses. When hormone therapy causes a drop in libido, the sexologist can assist both the patient and couple in coping with the situation to avoid suffering, discouragement, and guilt.
The social worker
The social worker focuses on the social well-being of the patient. The social worker works with the patient and his family and assists the patient with the procedures for obtaining financial assistance required during cancer treatments. The social worker also works with the healthcare team organize the patient’s discharge from the hospital with the help of community resources (CLSC, rehabilitation centres, etc.)
The spiritual advisor
The spiritual advisor offers religious and spiritual support to people who are hospitalized and their loved ones.
Working with your healthcare team
It is very important to keep your healthcare team up‑to‑date on your mood as you progress through your cancer treatment. Open and honest communication about how you’re feeling is imperative if you want your healthcare team to be able to help you.
Additional Information - Side effects
Living with permanent erectile dysfunction
Managing permanent ED after prostate cancer is delicate. Discover strategies to cope with it.
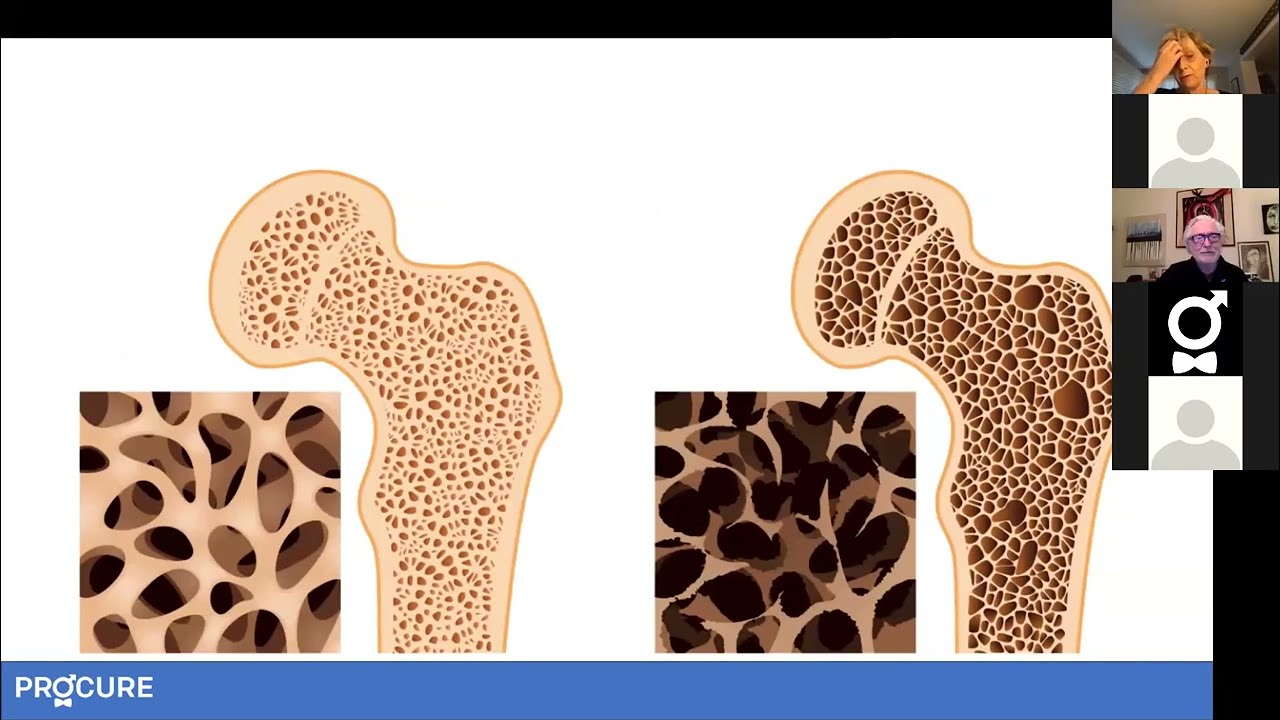
Hip fracture? No thank you! Male bone health
Dietary and physical adjustments can improve bone health and reduce the risk of fractures.

Nutrition during and after your treatment
Adjustments you can make to your diet or whether you have or are being treated with radiation therapy, hormone therapy, or chemotherapy with clinical dietitian.

Living Fully, Drinking Moderately
Benefits of Drinking Less and Flavourful Recipes to Guide You Are you aiming for a healthy start to the year by reducing or completely abstaining from alcohol? It can be challenging, especially when many of our social activities revolve around drinking, such as “Happy Hours” or going to a bar with friends for a sporting […]

Rediscovering Well-being After Treatments
After completing treatments, people often feel a mix of concern and relief. The main focus during this transition is rediscovering well-being.

Do you have a curved penis?
Is your penis curved? Does it curve to the left, right, upward, or downward? You have a curved penis and you or your partner want to know why?

Orgasm without erection?
It is entirely possible for a man to achieve orgasm without an erection or penetration and there are several ways to achieve this.

Simple and easy-to-make healthy recipes
Regardless of the season, why not take the opportunity to cook simple and easy-to-make healthy recipes that are rich in nutrients beneficial for your heart and prostate?!

Fresh start with new habits
We don’t have to wait until January 1st to make a fresh start and adopt new habits. This decision can be made at any time during our life.

Does warm milk help you sleep better?
Can a glass of warm milk help you sleep better in the arms of Morpheus? The Rumor Detector wondered if the research has confirmed this.

I am a little bit diabetic
My doctor informed me that I am a little bit diabetic and that I will have to make important changes to my lifestyle.

Caring for your bones in 5 points
Nicknamed “the silent thief” due to the absence of symptoms, osteoporosis is often only detected at a more advanced stage following a fracture.
Sources and references
Last medical and editorial review: April 2024. See our web page validation committee and our collaborators by clicking here.

