Chemotherapy related effects
- Side effects
- Chemotherapy related effects
- Overview
- Most common side effects

Chemotherapy related effects
Chemotherapy related effects
Chemotherapy is sometimes referred to as the treatment that may make you feel sick in order to get better. Most people fear its side effects, partially because people only hear about the most extreme side effects.
Keep in mind that not everyone experiences serious side effects and that any discomfort is usually temporary.
Side effects vary in type and severity from person to person and from medication to medication. Damage to normal, healthy cells is the cause of side effects. To learn more, see our section on side effects or visit chemoready.ca, a specialized website on the subject.
Chemotherapeutic agents
- Docetaxel (Taxotere): Side effects associated with docetaxel use include neutropenia (decrease in white blood cells), fatigue, hair loss, diarrhea, neuropathy (nerve disorder), limb edema (swelling of tissues due to water retention), and nail dystrophy.
- Cabazitaxel (Jevtana): Side effects associated with its use include fatigue, diarrhea, hematuria (blood in the urine), anemia, neutropenia (decrease in white blood cells), hair loss, and limb edema (swelling of tissues due to water retention).
Hormone therapy drugs used in combination
- Abiraterone (Zytiga): Presents more specific adverse effects such as hypertension, water retention and edema (swelling of tissues due to water retention), fatigue, urinary tract infection, cardiac arrhythmia, and liver damage.
- Enzalutamide (Xtandi): Can lead to headaches, hot flashes, hypertension, back pain, respiratory tract infection, anxiety, diarrhea, fatigue, seizures, blood in the urine, and edema.
- Apalutamide (Erleada): Can cause hot flashes, joint pain, diarrhea, nausea, fatigue, loss of appetite, itching, and weight loss.
- Darolutamide (Nubeqa): May cause pain, unusual fatigue, or skin rash and redness.
Some men may experience all the side effects, while others may experience only a few or none at all. Others may experience different side effects.
Increased risk of infection
You will be asked to monitor your temperature regularly and to inform your doctor if you notice wounds that are not healing. The increased risk of infection is due to the decrease in your white blood cells (neutropenia).
What you can do
- Wash your hands often and/or use an antiseptic gel.
- Immediately clean any cuts with soap and water, and apply antiseptic.
- Avoid crowds and people with infections.
- Trim your nails carefully to avoid cuts.
- Use an electric razor to shave.
- Wash and peel raw fruits and vegetables.
- Do not eat undercooked meat.
- Do not clean cat litter boxes or bird cages.
Fatigue
If you feel tired, take care of yourself emotionally and physically. Limit the number of visitors or the duration of visits and rest several times during the day.
What you can do
- Physical activity can help cope with fatigue.
- Try to conserve your energy by delegating as many tasks as possible or making them easier (e.g., sit down while preparing meals, get someone to drive you to your treatments).
Anemia
Chemotherapy causes anemia in some men. When the number of red blood cells or the hemoglobin concentration is low, the body tissues do not get enough oxygen. This results in fatigue and shortness of breath.
What you can do
- Iron supplements are provided in the form of tablets or directly intravenously, depending on tolerance and circumstances.
- The iron level can only be improved through diet when iron deficiency is due to an unreasonable diet. Eat a balanced diet. Follow your doctor’s and nurse’s instructions for appropriate nutrition and, if recommended, for nutritional supplements.
Gastrointestinal problems
Nausea and vomiting may occur within hours after your chemotherapy and usually last for about 24 hours. Medications can prevent these effects in many men.
Diarrhea may occur shortly after the start of your chemotherapy and may last up to two weeks after treatment.
What you can do
- Discuss it with your healthcare team. Medications may be prescribed.
- Ask to meet with a nutritionist if you haven’t already.
- Practice physical or relaxation activities (yoga, meditation) between treatments.
Mouth ulcers
Regular and thorough mouth hygiene can help prevent pain and reduce infection. The healthcare team provides guidance on the frequency of mouth cleaning and rinsing and on the products to use. Analgesics or special oral solutions may be necessary to relieve pain. A special mouthwash can help minimize them.
What you can do
- Avoid acidic, salty, sour, or spicy foods.
- Drink plenty of fluids. This will help heal the ulcers.
- Remove your dentures frequently to rest your gums.
- Keep your mouth moist. If your mouth is dry, suck on an ice pop or hard candy.
Nail changes
Nail changes are common during chemotherapy and can affect fingernails and toenails. Your nails may darken, yellow, become brittle, crack, develop ridges, or partially separate from their beds. Nail darkening usually fades a few months after chemotherapy.
What you can do
- Use a cuticle cream rather than tearing or cutting them.
- Protect your nails by wearing gloves when washing dishes, gardening, or doing other household chores.
- Most men do not have late effects after chemotherapy, but some may experience numbness or tingling in the hands and feet.
Additional Information - Side effects
Advanced prostate cancer treatments strategies
Strategies for treating advanced cancer have significantly evolved, offering new options and hope for patients.
Prostate Cancer Study Results Summaries (2023 ASCO-GU)
Summary of clinical trial results on promising prostate cancer research.
Advanced Prostate Cancer Triple Therapy Study Results (2023 ASCO-GU)
Clinical trial results on triple therapy for advanced hormone-sensitive prostate cancer.
Expert Opinion: Prostate Cancer and Hormone Therapy
What you need to know about hormone therapy and how to manage the side effects of this treatment.
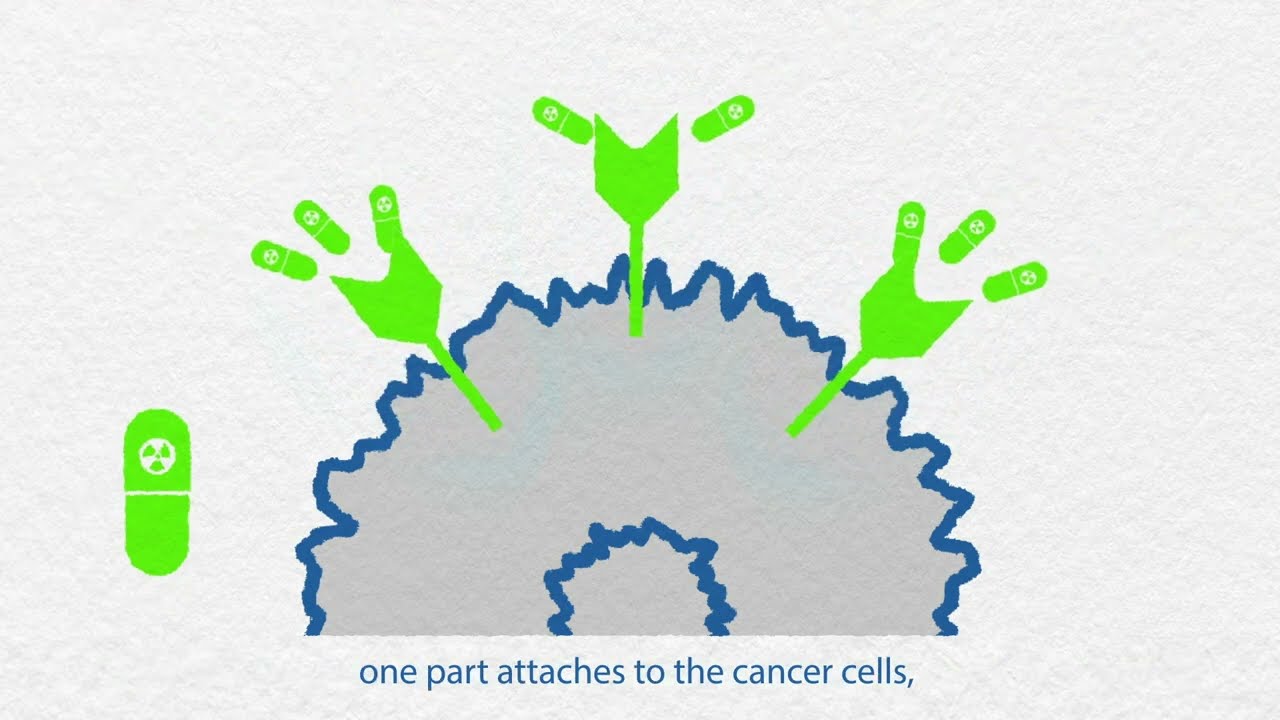
Prostate cancer and nuclear medicine
What about nuclear medicine? Is it suitable for your situation?
Nuclear imaging technologies
Has your doctor suggested prostate imaging tests? Explore options like PSMA PET scans.
Targeted therapy and inherited mutations
If you have a specific genetic mutation, you could benefit from new targeted treatments.
States of prostate cancer following treatment
Do your recent tests show an increase in PSA levels? It could indicate a recurrence.
The role of hormone therapy
Has your doctor recommended hormone therapy? This video is for you!
Advanced prostate cancer treatment strategies
Strategies for treating advanced cancer have significantly evolved, offering new options and hope for patients.
Advanced prostate cancer treatment
Advanced prostate cancer encompasses various conditions, including metastatic, recurrent, and hormone-resistant forms, each raising different questions and concerns.
When prostate cancer comes back
A recurrence is when the cancer returns after treatment. The main question is, “What’s next?”
How to treat advanced prostate cancer
Advanced prostate cancer encompasses various conditions, including metastatic, recurrent, and hormone-resistant forms, each raising different questions and concerns.
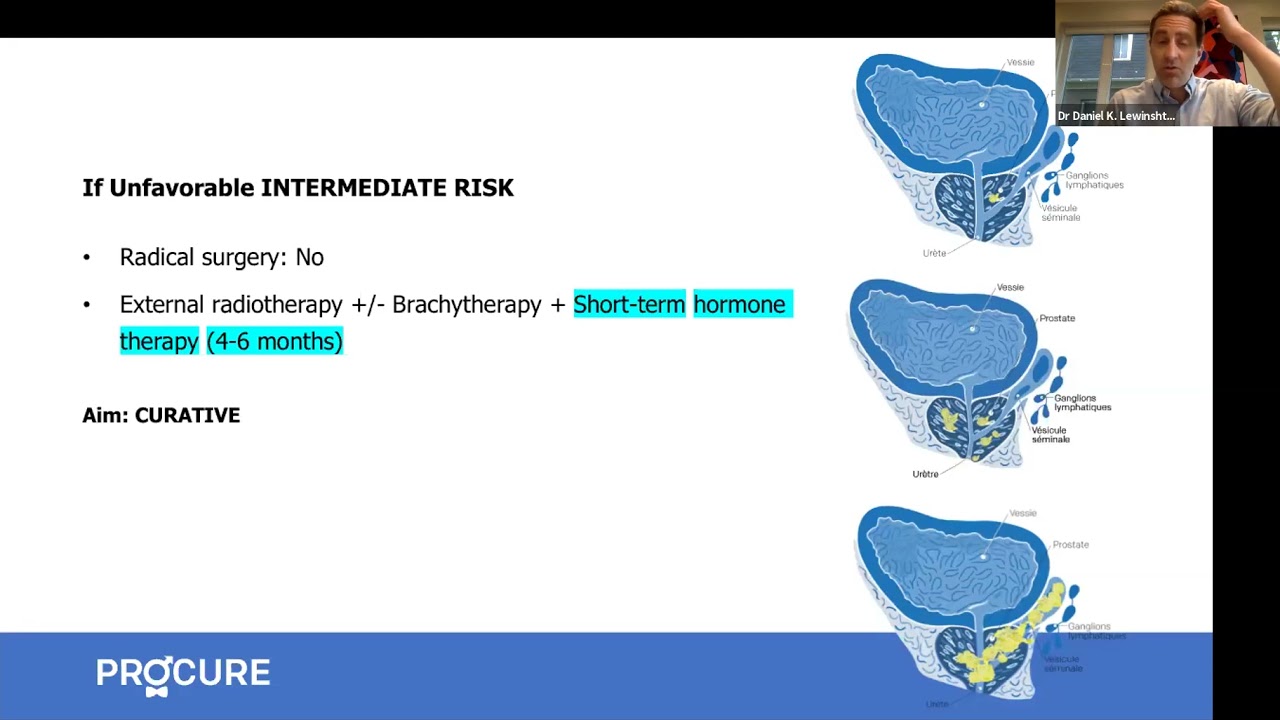
All about hormone therapy
Hormone therapy can reduce tumor size, control cancer, and prolong life. Is it the right treatment for your cancer?
Q-A – New therapies for advance prostate cancer
In this interview, we answer patients’ questions about new therapies for advanced prostate cancer.

Advanced cancer: Factors influencing life expectancy
Being diagnosed with advanced prostate cancer can be overwhelming and frightening. It’s natural to have many questions about your prognosis and what the future holds. One of the key concerns for many patients is understanding their life expectancy. In this article, we’ll explore the factors that can impact life expectancy in advanced prostate cancer and […]

Orchiectomy? Never heard of that word!
Orchiectomy, a form of hormone therapy, involves surgically removing the testicles, depriving the cancer of testosterone.

Food tastes funny…!
I feel like one of the worst effects was losing my taste buds. Everything I tried to eat tasted funny. So why food tastes funny?
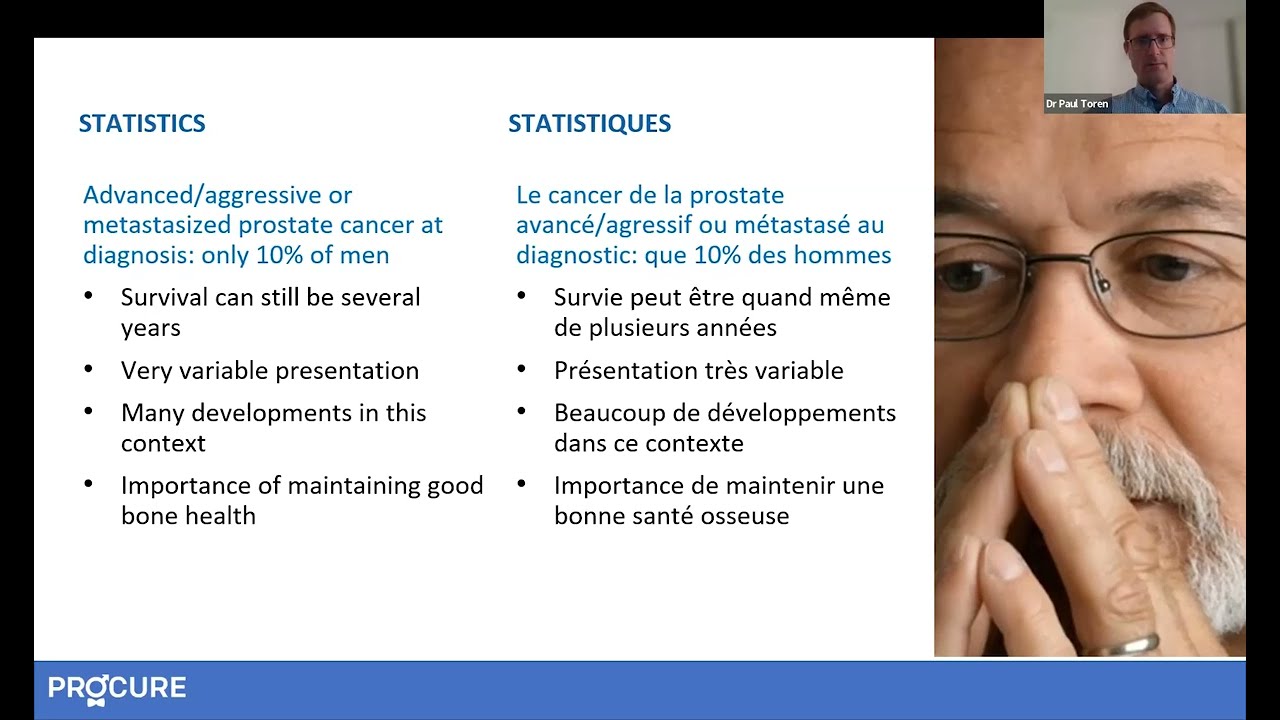
Advanced prostate cancer-What should I know?
Advanced prostate cancer-What should I know? The term advanced prostate cancer does not describe just one type of disease, but several. It can be locally advanced, recurrent, metastatic, or resistant to castration. These terms are probably unfamiliar to you and can raise many questions. Here are 5 things you should know Your cancer has returned? […]

When hormone therapy significantly increases overall survival…
The arrival of next-generation hormone therapy to treat non-metastatic castration-resistant prostate cancer provides a significant opportunity for men and their families. Non-metastatic castration resistant prostate cancer treatment NUBEQA® (darolutamide) significantly improves overall survival with a favourable safety profile in men with non-metastatic prostate cancer. Source: Bayer Canada Press Release MISSISSAUGA, ON, June 16, 2020 – Data […]

Can you have a good life despite advanced cancer?
Today, many patients now have access to more than one drug that can help them live longer and improve their quality of life, despite living with advanced cancer. I was diagnosed at the age of 65 and I have been living with my prostate cancer for 20 years. And to all the men who have this […]

Welcome life… Serge’s story
Welcome life… The second part of Serge’s testimony “In my previous testimony, Alone against my diagnosis, I mentioned that when my prostate cancer was announced, a very aggressive cancer, my partner at the time had ended our relationship, the disease – especially cancer – not being her cup of tea. So I found myself in front […]

Alone against my diagnosis… Serge’s story
Alone against my diagnosis… Just like Martin, Serge learns that he has prostate cancer in the prime years of his life, that is to say at the beginning of his fifties (yes age… is relative). What you need to understand is that men who receive a prostate cancer diagnosis are usually much older, well in their sixties […]
You no longer respond to your hormone therapy?
As you know, hormone therapy is mainly used when first treatments fail or when a patient is not a candidate for radical surgery or radiotherapy. On occasion, it can be combined with other treatments, such as radiotherapy. As you also know, hormone therapy may be slowing the growth of prostate cancer, but it cannot cure […]
Sources and references
Last medical and editorial review: April 2024. See our web page validation committee and our collaborators by clicking here.

