With your urologist
- All about screening
- With your urologist
- Consultation
- Expectations and results
With your urologist

Meeting with your urologist
A urologist is a doctor specializing in genitourinary system disorders. Like your doctor, your urologist will be interested in your:
- Symptoms
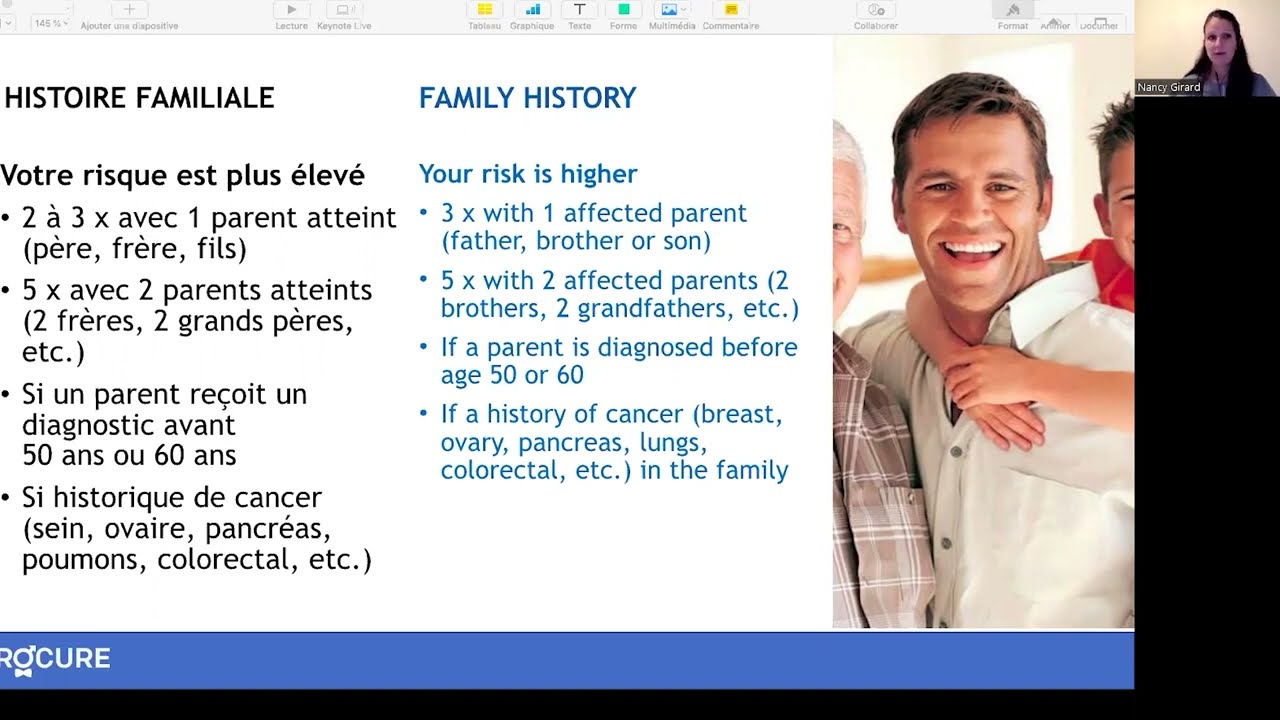
- Family history
- Medical history
La prostate est constituée de cellules:
- glandulaires qui sécrètent les liquides pour l’éjaculation
- musculaires qui participent à l’évacuation de votre sperme au cours de l’éjaculation
- fibreuses qui maintiennent la structure de votre glande
Your urologist will probably ask you to retake certain tests and exams that you were already given, but he will also ask you to undergo a number of other tests that will help in determining your diagnosis. It is important to know whether you have prostate cancer or benign prostatic hyperplasia. These tests can include:
- A physical examination;
- A digital rectal exam (DRE);
- A PSA test;
- A urine analysis;
- A urine flow test: this test checks to make sure that the bladder and sphincter that is responsible for holding the urine in the bladder is working. For this test, you will need to urinate into a special funnel connected to an instrument that calculates the speed of urination;
- A bladder ultrasound: this ultrasound evaluates the volume of urine remaining in the bladder after urination, and the possible urinary obstruction due to pressure from the prostate; A transrectal ultrasound (TRUS) of the prostate;
- A magnetic resonance imaging of the prostate (MRI): Allows visualization of the prostate and possibly cancerous lesions in it;
- A prostate biopsy.
Transrectal ultrasound (TRUS)
Why? The transrectal ultrasound (TRUS) of the prostate measures the size of the prostate and identifies abnormal regions to be biopsied. It is standard for a biopsy to be performed at the same time as a TRUS which helps guide the biopsy needles during sample collection.
How? For a transrectal ultrasound, you will be asked to lie on your side with your knees brought up to your chest while a lubricated probe is inserted into your rectum. This probe emits sound waves that bounce off the prostate and surrounding tissues back into the sensor. The machine will then show an image of the prostate and the surrounding area on a computer screen. The TRUS does not last longer than a few minutes and does not require any special preparation. It is not painful, but some men find it unpleasant.
Prostate biopsy
Why? Abnormalities detected during a digital rectal exam and a high PSA level often lead to a prostate biopsy. This procedure consists of taking small tissue samples of your prostate in order for the pathologist to examine them under a microscope to determine if they are cancerous or not. If cancer is detected, the pathologist will use the same samples to calculate your Gleason Grade score.
How? A prostate biopsy is usually performed during a transrectal ultrasound (TRUS biopsy). The images taken with the ultrasound help guide a fine needle to the areas selected for sampling. The spring-loaded needle is attached to the ultrasound probe and enters the prostate through the rectum. Usually between 6 – 12 (sometimes more) prostatic tissue samples are obtained and the entire procedure lasts about 10 minutes. A local anesthetic can be used to numb the area and reduce any pain.

A transrectal ultrasound (TRUS) of the prostate done without a biopsy cannot confirm the presence of cancer. If your urologist detects an abnormality following a TRUS, a biopsy is needed to confirm the prostate cancer diagnosis. It takes about four weeks to get the biopsy results because the pathologist needs to examine the samples under a microscope before giving his report.
Presence of cancer
- If the pathologist finds cancer in the samples, he will assess the aggressiveness of the cancer by giving it a Gleason grade.
- You will discuss possible treatments with your urologist who may recommend other complementary tests in order to determine how far your cancer has progressed.
Absence of cancer
- The fact that the pathologist did not find any cancer in your samples can be reassuring. However, it is possible that the biopsy needle simply missed the cancerous areas and you do in fact have cancer.
- If your urologist suspects that you have cancer, he may have you do a second transrectal biopsy or another type of prostate biopsy.
- Otherwise, regular prostate checkups, including the PSA test, digital rectal exam (DRE), and magnetic resonance imaging (MRI), may be the preferred route.
Additional Information - All about screening
Is prostate cancer hereditary?
Understanding the hereditary and genetic aspects of this disease can provide valuable information to both individuals affected and their families.
Genetics and prostate cancer
Do you have a family history of cancer? Your doctor might recommend genetic screening.
Symptoms, risk and screening
Are you over 50 or experiencing urinary problems? Discover why early screening for prostate diseases is important.
From prostate to screening
Learn about the role of your prostate, related diseases, symptoms to watch out for and risk factors.
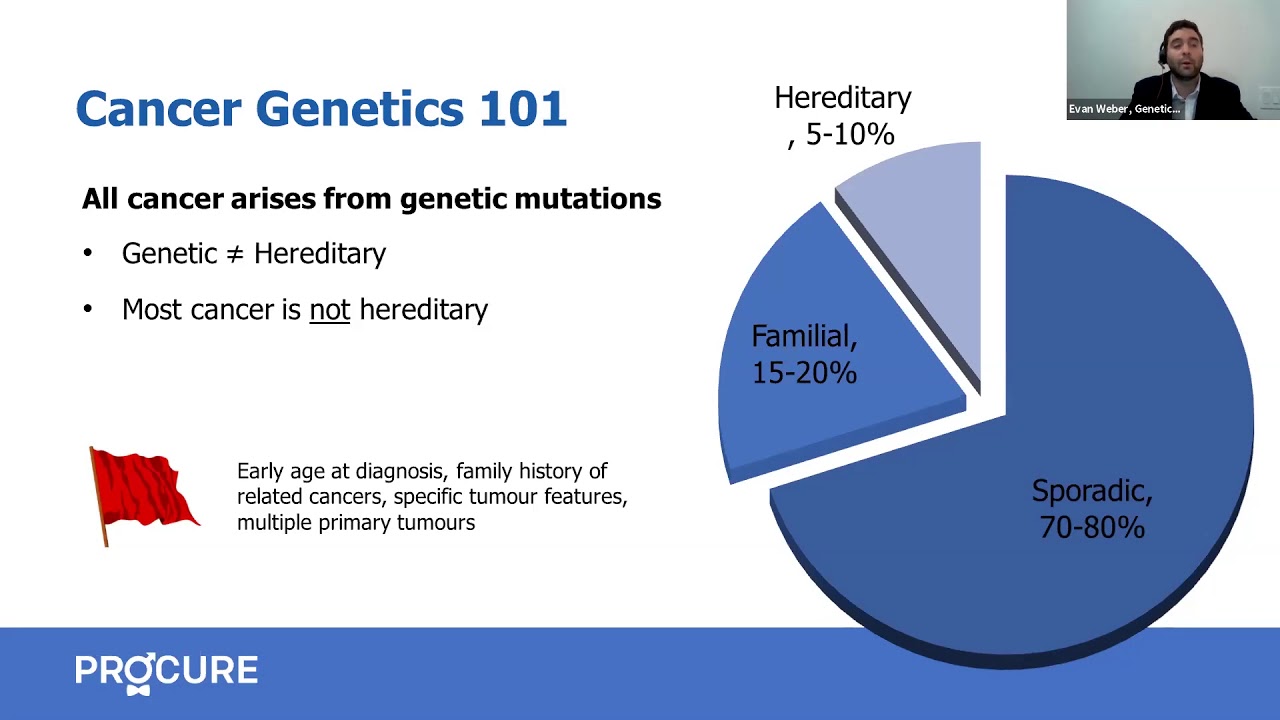
Genetic predisposition to prostate cancer
Although rare, some hereditary genetic mutations can increase your risk of prostate cancer.

Do you have a curved penis?
Is your penis curved? Does it curve to the left, right, upward, or downward? You have a curved penis and you or your partner want to know why?

Can I prevent BRCA-related prostate cancer?
How to prevent BRCA-related prostate cancer? Can I have a radical prostatectomy or a proactive treatment to prevent prostate cancer?

What is a genetic mutation?
Do you have a significant family history of cancer? Is there a link between prostate cancer and a genetic mutation?
My balls hurt!
While sore balls are a common experience and usually no cause for concern, it’s important to familiarise yourself with symptoms in case it’s a sign of something serious.

I feel a heaviness in my underwear
I feel a heaviness in my underwear and I know it’s not normal… And sure enough, you notice your balls are much bigger than usual.

What women should know about prostate cancer
As a woman, you might think that prostate cancer is not your concern because you don’t have a prostate. However, prostate cancer is the most common cancer in men.

Why a health check?
The short answer to this question is to assess your health. This is the starting point for a health check. Could we be in the presence of potential undetected diseases?

10 signs that encourage you to see a doctor
There are many reasons why men will be referred to a specialist, and if you experience any of the following symptoms you should see a family doctor. Here are 10 signs that encourage you to consult. You should also know that unless you go to a private clinic, you cannot consult a specialist directly, such as […]

From your prostate to screening in 5 points
From your prostate to screening in 5 points. Gentlemen, are you over 50 years old, or have you been having urinary problems for some time now? Several diseases can affect your prostate, and it’s important to detect them early. Let’s take a closer look. The size of a walnut, the prostate is located just below […]
Sources and references
Last medical and editorial review: April 2024. See our web page validation committee and our collaborators by clicking here.

