Hormone therapy related effects
- Side effects
- Hormone therapy related effects
- Short to medium-term effects
- Long-term effects
- Tumoral flare and orchidectomy

Hormone therapy related effects
Hormone therapy related effects
No matter what prostate cancer treatment you undergo, there is always the possibility of developing side effects. However, not everyone gets side effects; if you do get side effects, not everyone feels them in the same way. Side effects of hormone therapy are dependent on the following:
- The type of hormone therapy (surgery or drugs)
- Your medication dose and duration (how long you take it for)
- Your overall health
- The side effects, although transient, can be difficult to manage, and some patients are tempted to stop treatment. However, it is important to bear in mind the major therapeutic impact of hormone therapy. In addition, there are usually ways to manage them and help the patient overcome them. Here is a guide to inform you about this treatment and provide you with some helpful tips for managing your symptoms and taking care of yourself.
- Do not hesitate to talk about all of your side effects with your doctor during your follow-up visits.
Decrease in libido
The decrease in hormone production will result in the loss of sexual desire (libido), whether you have undergone surgical or medical castration. After more than two years of continuous medication, testosterone levels may never return to normal. Medications that facilitate erection are not of much help when there is no libido.
Nevertheless, despite the absence of sexual desire, patients may still resort to medical means that allow for an erection (see below). However, in most cases, your sexual desire gradually reappears once the treatment is completed.
What you can do
- Discuss it with your doctor. You may need to consult a sexologist, either alone or with your partner. These professionals can help couples strengthen their bonds, communicate, and explore different ways of being intimate. For more information, we invite you to watch our conference on sexuality by clicking here.
Erectile dysfunction (inability to achieve an erection)
- This is a very common side effect of hormone therapy due to the loss of libido. It can be permanent with the removal of both testicles. Otherwise, it persists throughout hormonal treatment. It may take 3 to 12 months after hormone therapy to regain erectile capacity. If erectile capacity does not return on its own, treatments may be necessary.
- Your erectile capacity after hormone therapy depends on your sexual function before treatment, your age, and your overall health.
What you can do
- Your doctor will prescribe treatment to help you regain your erectile capacity and achieve a satisfying sex life after your treatment.
- Treatments include oral medications such as tadalafil, sildenafil, vardenafil; the MUSE pill, penile injection, vacuum pump, or penile implant through surgery.
For more information on erectile dysfunction, see our section on side effects.
Hot flashes
Although this discomfort is typically associated with women, hot flashes can occur in about 50 to 80% of men undergoing hormone therapy. It is a sudden sensation of heat in the face and chest that then spreads to the rest of the body in waves, lasting 2 to 30 minutes. You may also sweat, flush, feel your heart pounding, or feel anxious. The exact cause of hot flashes is unknown, but it may be related to how hormones interact with the hypothalamus, part of your brain that controls body temperature.
Hot flashes generally disappear when your body adjusts to the treatment or when the treatment is stopped, but there are several measures you can take on a daily basis to better manage them.
What you can do
- Drink fluids to stay hydrated, preferably cool non-alcoholic and caffeine-free beverages;
- Avoid spicy foods;
- Wear breathable clothing (e.g., 100% cotton clothing);
- Layer clothing so you can remove layers when you feel too hot; Keep good airflow in the house by opening windows and using fans;
- Take a shower or bath with lukewarm water rather than hot;
- Place sponge towels on your mattress and pillows if you tend to sweat excessively in bed;
- Practice slow, deep breathing when you feel the onset of a hot flash, or try relaxing activities like yoga or meditation.
- Discuss your hot flashes with your doctor if they are unbearable, as there are treatments that can help you.
Weight gain and muscle loss
Weight gain and muscle loss are common side effects of hormone therapy. Increased adipose tissue causes weight gain, and muscle tissue loss leads to decreased strength.
What you can do
- You can mitigate your weight gain and muscle loss through a healthy diet and physical activity.
- You can also seek the help of a nutritionist and kinesiologist (physical activity specialist) for additional support. Discuss this with your doctor, nurse, or CLSC social worker.
Fatigue
Fatigue makes a person more tired than usual and can interfere with daily activities and sleep. Fatigue may diminish over time. It is also possible that it will persist well after hormone therapy is completed.
What you can do
- Physical activity can help cope with fatigue. For more information on managing fatigue, see our section on side effects.
Concentration difficulties, irritability, or impatience
You may feel more emotional, expressive, angry, or irritable. You may also be more distracted and forgetful.
What you can do
- Keep a journal to help identify disruptive events and triggers;
- Start a conversation with a trusted person to help you put things into perspective;
- Discover activities and hobbies that make you feel good (e.g., music, reading, pet, outdoor activity, etc.);
- Develop strategies to cope with stress (e.g., breathe slowly, recognize your limits, take a moment to pause).
Swelling or tenderness of the breasts
Breast swelling in men is called gynecomastia. It is a common side effect of prostate cancer hormone therapy, especially when an oral anti-androgen such as bicalutamide is administered.
What you can do
- Discuss this side effect with your doctor.
Loss of bone density (osteoporosis)
Osteoporosis is a late side effect that may occur with certain hormonal medications (LH-RH). Bone mineral content assessment can determine the risk level.
What you can do
- Osteoporosis can be slowed or prevented through physical exercise and a healthy diet.
- Your doctor may prescribe products or medications to prevent or treat this complication: calcium, vitamin D, and even medications like bisphosphonates (if bones are very fragile due to age or the effects of hormone therapy).
Changes in masculine characteristics
- Hormone therapy causes hair loss and a decrease in testicle size. Men taking LH-RH analogs notice that their scrotum loses volume over time.
Depression
Hormone therapy for prostate cancer sometimes causes depression and changes in emotional stability.
What you can do
- Depression can be treated with antidepressants. To learn more about depression and how to recognize signs, see our section on side effects.
Anemia
Hormone therapy causes anemia in some men. When the number of red blood cells or the concentration of hemoglobin is low, the body tissues do not get enough oxygen. This results in fatigue and shortness of breath.
What you can do
- Iron supplementation is provided through tablets or directly intravenously, depending on tolerance and circumstances.
- Iron levels can only be improved through diet when iron deficiency is a result of an unreasonable diet.
Increased risk of cardiovascular diseases
This is because hormone therapy leads to weight gain, reduced exercise capacity, and increased blood levels of lipids and glucose. It is important to monitor your risk of heart disease and try to prevent or correct these diseases as much as possible. In fact, there are now two information sheets, one for you as a patient and one to give to your family doctor.
You should download and print them. If you don’t have a printer, contact us at 1 855 899-2873. We will send them to you by mail. The sheets are important because they highlight your role as well as that of your family doctor in reducing your risk of heart attack or stroke.
Information sheet for you (blue) and for your family doctor (purple)
Increased risk of developing metabolic syndrome
Hormone therapy decreases your cells’ sensitivity to insulin. It also causes an increase in your adipose tissue and a decrease in your muscle mass. These effects increase the risk of diabetes, dyslipidemia (e.g., high cholesterol levels), obesity, hypertension, etc. in men receiving hormone therapy.
What you can do
- Monitor your weight gain, diet, and get moving!
Tumoral flare reaction
The administration of LH-RH analogues initially causes a temporary increase in testosterone levels lasting about a week. This increase can temporarily worsen your symptoms; this is called a tumoral flare reaction. During this reaction, you may experience more urinary problems or bone pain.
Your doctor will prescribe an anti-androgen such as Casodex. Administered orally in pill form, anti-androgens block the action of androgens (male sex hormones) for a period of time to reduce flare symptoms.
Side effects related to orchidectomy
Surgical castration causes very few complications. Typically, postoperative pain, swelling of the scrotum, and bleeding from the wound are minimal. As with any surgical procedure, there may be an infection at the incision site. This infection will then be treated with antibiotics.
This surgery results in permanent side effects, including erectile dysfunction and decreased libido due to low testosterone levels.
Additional Information - Side effects
Advanced prostate cancer treatments strategies
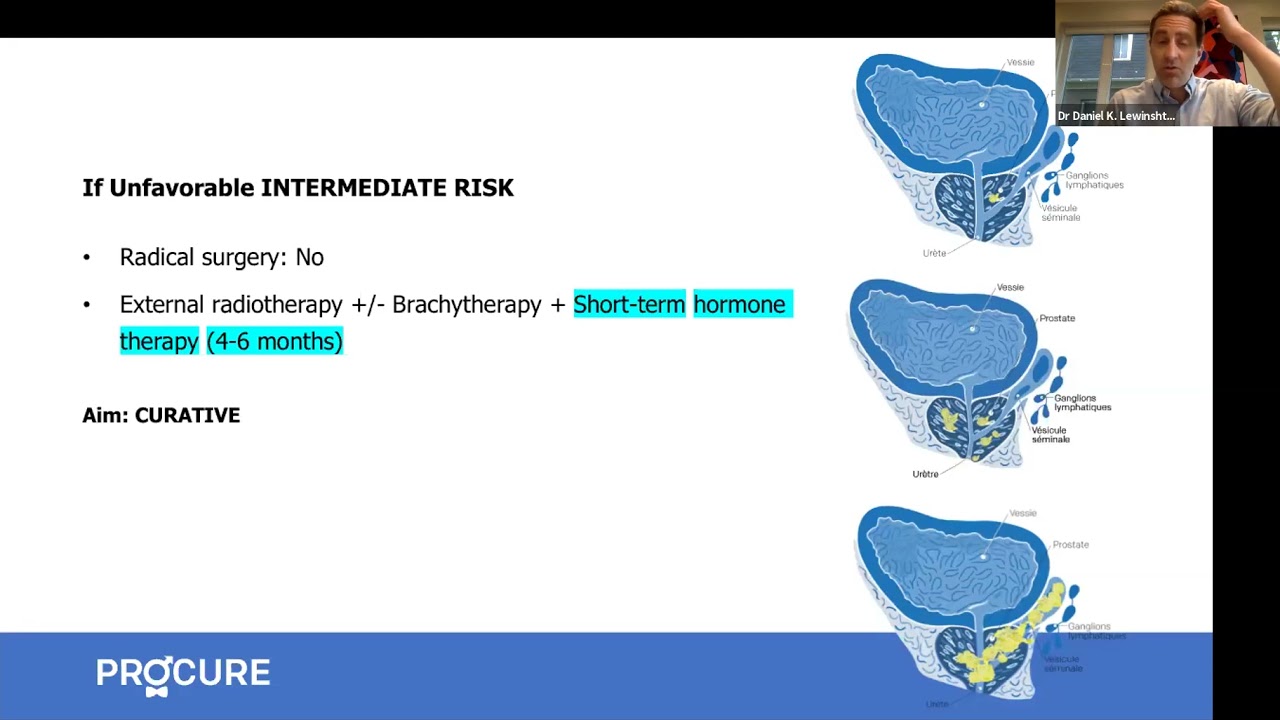
Strategies for treating advanced cancer have significantly evolved, offering new options and hope for patients.
Prostate Cancer Study Results Summaries (2023 ASCO-GU)
Summary of clinical trial results on promising prostate cancer research.
Advanced Prostate Cancer Triple Therapy Study Results (2023 ASCO-GU)
Clinical trial results on triple therapy for advanced hormone-sensitive prostate cancer.
Expert Opinion: Prostate Cancer and Hormone Therapy
What you need to know about hormone therapy and how to manage the side effects of this treatment.
Prostate cancer and nuclear medicine
What about nuclear medicine? Is it suitable for your situation?
Nuclear imaging technologies
Has your doctor suggested prostate imaging tests? Explore options like PSMA PET scans.
Targeted therapy and inherited mutations
If you have a specific genetic mutation, you could benefit from new targeted treatments.
States of prostate cancer following treatment
Do your recent tests show an increase in PSA levels? It could indicate a recurrence.
The role of hormone therapy
Has your doctor recommended hormone therapy? This video is for you!
Advanced prostate cancer treatment strategies
Strategies for treating advanced cancer have significantly evolved, offering new options and hope for patients.
Advanced prostate cancer treatment
Advanced prostate cancer encompasses various conditions, including metastatic, recurrent, and hormone-resistant forms, each raising different questions and concerns.
When prostate cancer comes back
A recurrence is when the cancer returns after treatment. The main question is, “What’s next?”
How to treat advanced prostate cancer
Advanced prostate cancer encompasses various conditions, including metastatic, recurrent, and hormone-resistant forms, each raising different questions and concerns.
All about hormone therapy
Hormone therapy can reduce tumor size, control cancer, and prolong life. Is it the right treatment for your cancer?
Q-A – New therapies for advance prostate cancer
In this interview, we answer patients’ questions about new therapies for advanced prostate cancer.

Do your medications cause erectile dysfunction?
Aside from prostate cancer treatments, if you experience erection problems such as erectile dysfunction, it’s crucial to understand that this can be related to various causes. Often, erectile dysfunction is triggered by reduced blood flow to the penis or issues affecting the nerves responsible for erection. These situations frequently arise from other health problems such […]

Vacuum erection devices: What you need to know
Vacuum erection devices (VEDs), or penile pumps, are a non-invasive solution for men experiencing erectile dysfunction (ED), particularly after radical surgery to treat prostate cancer. These devices can help restore erectile function, improving quality of life and intimacy. Let’s explore what to look for when buying a VED, the benefits of choosing a medical-grade device, […]

Living with permanent erectile dysfunction in 5 points
Living with permanent erectile dysfunction in 5 points outlines the essential considerations in navigating this reality. These tips serve as guiding principles to assist individuals, whether they are in a relationship or facing this situation alone. Healthcare professionals are here for you Sexuality is ever-present; it does not disappear with permanent erectile dysfunction. Consult healthcare […]

Sexuality and intimacy in 5 points
Sexuality and intimacy in 5 points addresses specific challenges and opportunities that may arise after treatment for prostate cancer.

Orgasm without erection?
It is entirely possible for a man to achieve orgasm without an erection or penetration and there are several ways to achieve this.

Food tastes funny…!
I feel like one of the worst effects was losing my taste buds. Everything I tried to eat tasted funny. So why food tastes funny?

I am a little bit diabetic
My doctor informed me that I am a little bit diabetic and that I will have to make important changes to my lifestyle.

Will the effects of hormone therapy disappear?
Hormone therapy is used to prevent your body from secreting or using testosterone. But what about the side effects of hormone therapy?

Why am I urinating my semen
If you are wondering why you urinate your semen, the answer is that you have what is called retrograde ejaculation.
Sources and references
Last medical and editorial review: April 2024. See our web page validation committee and our collaborators by clicking here.


