Your well-being
Your well-being
In this section dedicated to your well-being, we address various aspects of your health, whether they are mental, emotional, or physical. You will find practical advice and strategies to maintain optimal quality of life throughout your battle against prostate cancer.
The importance of healthy eating
Good nutrition is important at every stage of your prostate cancer journey. Clinical research suggests that a heart-healthy diet can lead to a better prognosis, while also protecting your heart health. Maintaining a healthy lifestyle – through diet and physical activity – can set you up for success by improving your energy, strength and overall health.
Following the Canadian food guide can help:
- Meet your vitamin, mineral and other nutrient needs
- Reduce your risk for heart disease
- Contribute to your overall health and energy
This guide shows how many servings of each food group men ages 51+ should aim to consume per day. For more information, see our Nutrition and healthy body section. Do not hesitate to speak to a dietitian or to a nutritionist and do not take supplements or natural products without talking to your doctor.
Servings for men
Vegetables and fruits (7-9 servings)
- Aim to eat at least one dark green and ne orange vegetable per day. Romaine lettuce, spinach and broccoli are examples of dark green vegetables. Sweet potatoes, carrots and squash work well as orange vegetables.
- Look for fruit and vegetables that are steamed, baked or stir-fried – and avoid those that are deep fried. It’s best to choose vegetables and fruits that are not prepared with lots of added salt, fat or sugar
- Choose whole fruits and vegetables more often than juice, to meet your daily servings goal.
Grain products (7 servings)
- Whole-grain products should make up at least half of your daily grain product servings. Look for whole grain options such as barley, brown rice, quinoa, oats, wild rice, whole grain breads and pasta.
- Compare nutrition facts – and choose grain products lower in salt, fat and sugar.
Milk and alternatives (3 servings)
- Choose lower fat milk products. For products made from milk (such as cheeses or yogurts), compare nutrition facts and select options that are lower in fat
- Drink milk every day. You should aim to drink 2 cups of milk per day to make sure you’re getting enough vitamin D. Choose either skim, 1% or 2% milks, or fortified soy beverages
Meat and alternatives (3 servings)
- Look for lean meats and alternatives that have limited added salt and fat. Remove skin on poultry and visible fat on meat. Bake, roast or poach prepared meats and alternatives. When choosing pre-packaged meats, compare nutrition facts and choose those with less sodium and fat
- Eat at least 2 servings of fish per week. For example, you could choose to eat herring, char, mackerel, salmon or trout
Making healthy choices
When choosing which foods to eat, it’s generally best to eat a diet that is:
Plant-based
Try to eat lots of fruit and vegetable servings. Beans, legumes and whole grains also work well.
Low in saturated fat
Try reducing or eliminating your intake of high fat meats, milk and other dairy products. Try limiting your consumption of butter, mayonnaise and baked goods.
High in fibre
Whole grain breads, oats, barley, quinoa and bulger are all high-fibre choices.
Low in simple sugars
Aim to limit your intake of candies, baked goods, and other foods made with simple sugars and refined flours.
Low in salt
Prepared foods can contain high levels of salt – so try to choose reduced-salt prepared meals, canned soups, snacks (unsalted or lightly salted nuts and chips) and condiments (reduced sodium soy sauce and ketchup). Using salt substitutes and using more herbs and spices while cooking can also help provide flavour without the added salt.
Tips for eating well
These tips can help you keep your body well-fueled:
Indulge in snacks
Eat smaller, more frequent snacks, every few hours, throughout the day. If appetite is an issue, don’t be shy about treating yourself to your favourite foods – your body may need the calories.
Eat more protein
Protein is important to help your cells grow and repair themselves. Try to eat more fish, poultry, lean red meat, eggs, dairy products and nuts.
Drink more water
Drinking water regularly is important for staying hydrated. You should aim to drink more water when you’re out in hot weather, or involved in physical activity.
Consider supplements
Different varieties of milkshakes, bars or powders are available at most pharmacies, and can be useful sources of protein and calories when you’re on the go or simply don’t have the time or energy to prepare a meal for yourself.
Work with your healthcare team
Since every case is different, your healthcare team may have specific guidance about what you should and shouldn’t eat. In particular, a dietitian plays an important role on your healthcare team to help create meal plans that meet your personal needs.
Staying active through treatment
During cancer treatment, it’s normal to not feel much like exercising, but it’s recommended by doctors to be as active as possible during your treatment and recovery. Regular physical activity has been shown to:
- Improve your mood and self-esteem, and reduce stress and anxiety
- Boost your energy and strength
- Stimulate your appetite
- Help you sleep
- Help you manage side effects like fatigue, nausea and constipation
An important role of physical activity is helping to maintain a healthy body weight, which has been shown to improve your ability to tolerate cancer treatment and its side effects.
Ways to get moving
Each person’s needs for an exercise program will be unique, and you should always talk to your doctor before starting or changing your exercise program. However, in general you should aim to maintain endurance, strength and flexibility so that you can continue to do the things that you want to do.
Start slow
Something as simple as walking is a good start. As you feel more confident, increase how often, how fast or how far you walk.
Find your best time
Be active at the time of day when you have the most energy. If you can’t make it through one long session, break your activities up into several shorter ones separated by rests.
Share something new
If you’ve been putting off trying a new and different activity or hobby, now is the time to give it a try! Bring along a friend and share in the excitement of learning something new.
Make it part of your routine
The house still needs to be cleaned, the lawn still needs to be mowed, and the car still needs to be washed – these all count as exercise! Doing a little bit every day will help keep you productive and active.
Working with your healthcare team
As mentioned above, always check with your healthcare team before starting or changing your exercise program. Cancer treatment can put you at higher risk of injury and infection, so not every activity will be right for you. You may also speak to a physiotherapist about specific exercises you can do, depending on the types of treatment (e.g. surgery) you’ve had.
Recognizing changes in your mood
Cancer treatment, and especially an advanced prostate cancer diagnosis, are stressful and life-changing events. It’s normal to feel anxious, nervous or depressed.
Some of the symptoms of anxiety and stress include:
- Excessive worrying, or restlessness
- Trouble sleeping, tiredness and exhaustion, or excessive sleeping
- Muscle tension
- Fast heartbeat, trembling, chest tightness, high blood pressure, nausea, dizziness and shortness of breath
- Trouble concentrating, irritability or impatience
Some of the symptoms of depression, especially in older people, include:
- Feelings of sadness, emptiness, hopelessness, anger, irritability or frustration
- Problems with memory, concentration, confusion or personality changes
- Sleep problems
- Losing interest in going out and socializing
- Suicidal thinking
If you find that your symptoms are lasting most of the day, every day, for more than two weeks, you should talk to your doctor and get help.
What causes anxiety and depression?
It’s important to understand that it isn’t a sign of weakness or failure, or your inability to cope with your diagnosis. The triggers of anxiety and depression can be different for everyone.
Tips for managing your mood
knowledge is power
Some people feel less anxious knowing everything about their cancer treatment, while others get stressed out by all the details. Figure out where you’re most comfortable to help control treatment-related anxiety.
Identify your triggers
Use a journal to write down your feelings and help you identify the events that make you feel most anxious or depressed – then you can figure out how to deal with them. Remember to record the positive things, too!
Talk it out
Start by talking with just one person about your feelings – like a family member, friend or someone who’s had a similar cancer experience. All it takes is one conversation to open up and take steps towards feeling better.
Surround yourself with positivity
Whether it’s people, events or pets, surround yourself with the things that make you happiest and the activities you enjoy.
Eat well and be active
A healthy diet helps maintain proper nutrition, and exercise releases natural mood-boosters called endorphins. Try low-impact and stress-relieving activities like yoga.
Cut down on caffeine
As part of a healthy diet, watch how much caffeine (a stimulant) you consume in drinks like coffee, tea or cola. You can easily start cutting back by switching to a decaffeinated version of the same drink.
Working with your healthcare team
It’s very important to keep your healthcare team updated on your mood as you progress through your cancer journey. Open and honest communication about how you’re feeling is key to them being able to help you.
Understanding your role
You may be family or a friend. Your loved one with cancer may be older, younger, a sibling or a coworker. You may be a spouse or partner. All of these things affect how you relate to your loved one, and the kind of support that you’re able to provide.
It’s important to understand your own strengths and weaknesses, and if needed build a team of caregivers with complementary strengths to help share the burden. In general, people with cancer may need three types of support:
- Emotional: Listening, providing comfort, encouraging sharing of feelings and providing company
- Practical: Helping with personal care, making appointments and travel
- Financial and legal: Helping find assistance for the cost of treatment, arranging wills and reviewing legal concerns
Things you can do
Within each of these three categories there are many things that you can do to help your loved one. Some useful ways to provide assistance include:
- Helping them live as normally as possible: When time is precious, it’s important to help them prioritize spending time on the activities they enjoy the most, with the people who matter most.
- Helping with visits to the doctor: Taking notes at appointments, organizing medical information, tracking symptoms and sharing them with the healthcare team.
- Helping with insurance and reimbursement: Collecting receipts, filling out forms and submitting them to insurance providers as needed.
Caring for yourself, too
Caregiver burnout is a serious problem that’s difficult to notice when you’re focusing all of your attention on your loved one – but you need to remember to look after yourself, too.
- Watch for the symptoms of depression
- Find “you time” to rest, focus on yourself and do something you enjoy
- Get a good night’s sleep every night, or take naps. It helps manage your stress levels
- Be physically active. This can help you to stay physically well and avoid getting sick, allowing you to continue to support your loved one
Other pages that might interest you
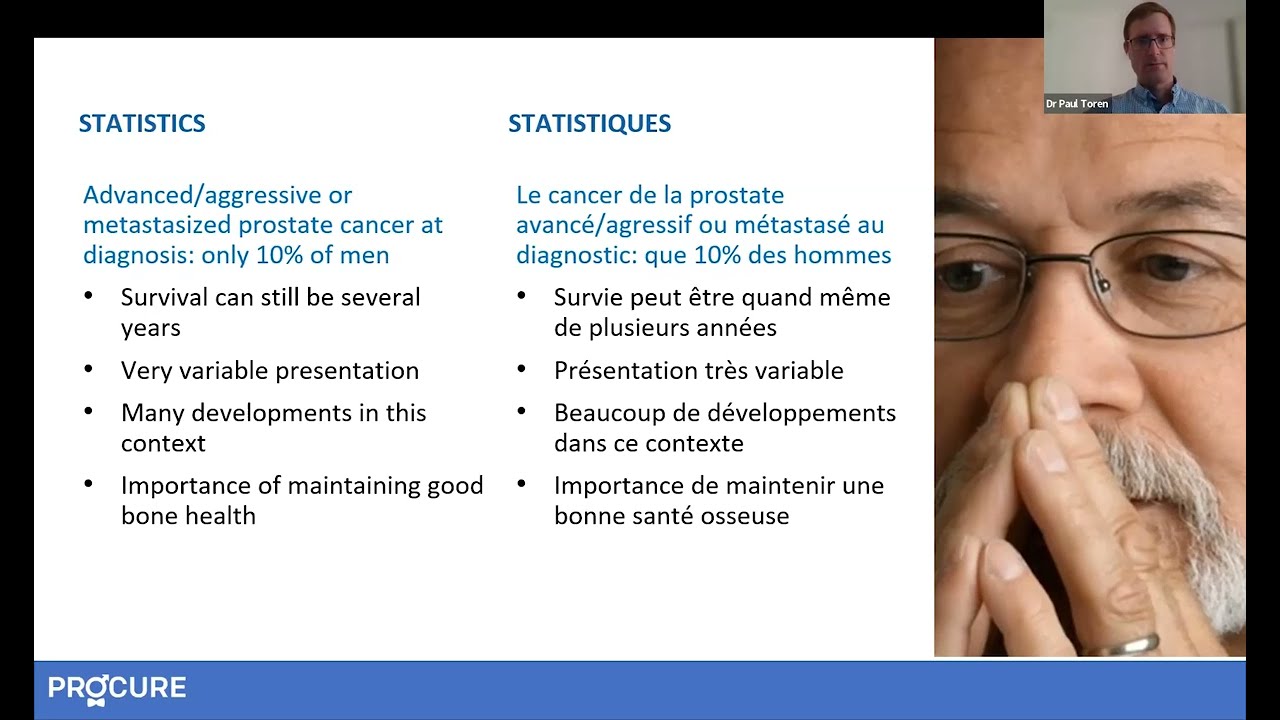
Additional Information - I have advanced cancer
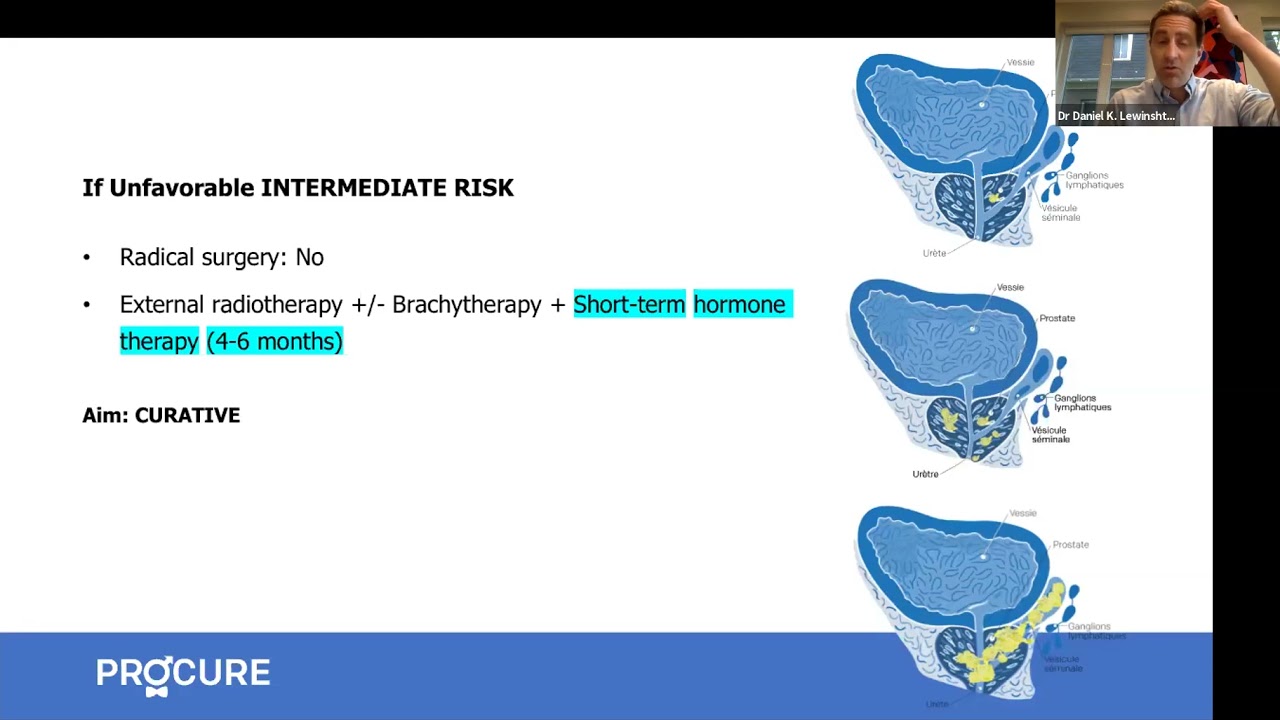
Advanced prostate cancer treatments strategies
Strategies for treating advanced cancer have significantly evolved, offering new options and hope for patients.
Prostate Cancer Study Results Summaries (2023 ASCO-GU)
Summary of clinical trial results on promising prostate cancer research.
Advanced Prostate Cancer Triple Therapy Study Results (2023 ASCO-GU)
Clinical trial results on triple therapy for advanced hormone-sensitive prostate cancer.
Expert Opinion: Prostate Cancer and Hormone Therapy
What you need to know about hormone therapy and how to manage the side effects of this treatment.
Prostate cancer and nuclear medicine
What about nuclear medicine? Is it suitable for your situation?
Nuclear imaging technologies
Has your doctor suggested prostate imaging tests? Explore options like PSMA PET scans.
Targeted therapy and inherited mutations
If you have a specific genetic mutation, you could benefit from new targeted treatments.
States of prostate cancer following treatment
Do your recent tests show an increase in PSA levels? It could indicate a recurrence.
The role of hormone therapy
Has your doctor recommended hormone therapy? This video is for you!
Advanced prostate cancer treatment strategies
Strategies for treating advanced cancer have significantly evolved, offering new options and hope for patients.
Advanced prostate cancer treatment
Advanced prostate cancer encompasses various conditions, including metastatic, recurrent, and hormone-resistant forms, each raising different questions and concerns.
When prostate cancer comes back
A recurrence is when the cancer returns after treatment. The main question is, “What’s next?”
How to treat advanced prostate cancer
Advanced prostate cancer encompasses various conditions, including metastatic, recurrent, and hormone-resistant forms, each raising different questions and concerns.
All about hormone therapy
Hormone therapy can reduce tumor size, control cancer, and prolong life. Is it the right treatment for your cancer?
Q-A – New therapies for advance prostate cancer
In this interview, we answer patients’ questions about new therapies for advanced prostate cancer.

Advanced cancer: Factors influencing life expectancy
Being diagnosed with advanced prostate cancer can be overwhelming and frightening. It’s natural to have many questions about your prognosis and what the future holds. One of the key concerns for many patients is understanding their life expectancy. In this article, we’ll explore the factors that can impact life expectancy in advanced prostate cancer and […]

Orchiectomy? Never heard of that word!
Orchiectomy, a form of hormone therapy, involves surgically removing the testicles, depriving the cancer of testosterone.

Food tastes funny…!
I feel like one of the worst effects was losing my taste buds. Everything I tried to eat tasted funny. So why food tastes funny?
Advanced prostate cancer-What should I know?
Advanced prostate cancer-What should I know? The term advanced prostate cancer does not describe just one type of disease, but several. It can be locally advanced, recurrent, metastatic, or resistant to castration. These terms are probably unfamiliar to you and can raise many questions. Here are 5 things you should know Your cancer has returned? […]

When hormone therapy significantly increases overall survival…
The arrival of next-generation hormone therapy to treat non-metastatic castration-resistant prostate cancer provides a significant opportunity for men and their families. Non-metastatic castration resistant prostate cancer treatment NUBEQA® (darolutamide) significantly improves overall survival with a favourable safety profile in men with non-metastatic prostate cancer. Source: Bayer Canada Press Release MISSISSAUGA, ON, June 16, 2020 – Data […]

Can you have a good life despite advanced cancer?
Today, many patients now have access to more than one drug that can help them live longer and improve their quality of life, despite living with advanced cancer. I was diagnosed at the age of 65 and I have been living with my prostate cancer for 20 years. And to all the men who have this […]

Welcome life… Serge’s story
Welcome life… The second part of Serge’s testimony “In my previous testimony, Alone against my diagnosis, I mentioned that when my prostate cancer was announced, a very aggressive cancer, my partner at the time had ended our relationship, the disease – especially cancer – not being her cup of tea. So I found myself in front […]

Alone against my diagnosis… Serge’s story
Alone against my diagnosis… Just like Martin, Serge learns that he has prostate cancer in the prime years of his life, that is to say at the beginning of his fifties (yes age… is relative). What you need to understand is that men who receive a prostate cancer diagnosis are usually much older, well in their sixties […]
You no longer respond to your hormone therapy?
As you know, hormone therapy is mainly used when first treatments fail or when a patient is not a candidate for radical surgery or radiotherapy. On occasion, it can be combined with other treatments, such as radiotherapy. As you also know, hormone therapy may be slowing the growth of prostate cancer, but it cannot cure […]
Sources and references
Last medical and editorial review: April 2024. See our web page validation committee and our collaborators by clicking here.