Glossary
Glossary
A
Abdomen: the part of the body below the chest that contains organs like the intestines, the liver, the kidneys, the stomach, the bladder, and the prostate.
Ablation: reduction of; e.g., in the management of prostate cancer, hormonal ablation means the use of hormonal techniques to reduce the spread of prostate cancer cells and cryoablation means the use of deep freezing techniques to reduce the number of live prostate and prostate cancer cells.
Active surveillance: active observation and regular monitoring of a patient (DRE, PSA level and re-biopsy) without aggressive treatment until there is evidence of disease progression.
Acute prostatitis: prostate infection characterized by the sudden flare-up of severe symptoms such as high fever and a burning sensation when urinating.
Adenocarcinoma: a form of cancer that develops from a malignant abnormality in the glandular cells lining an organ such as the prostate; almost all prostate cancers are adenocarcinomas.
Adjuvant: added on; e.g., adjuvant hormone therapy is hormone therapy added on to another form of therapy.
Adrenal: the two adrenal glands are located above the kidneys; they produce a variety of different hormones, including sex hormones – e.g., adrenal androgens.
Adrenalectomy: the surgical removal of one or both adrenal glands.
Age-adjusted: modified to take account of the age of an individual or group of individuals; for example, prostate cancer survival data and average normal PSA values can be adjusted according to the ages of groups of men.
Alphablockers: pharmaceutical drugs that act on the prostate by relaxing certain types of muscle tissue; these pharmaceutical drugs are often used in the treatment of BPH.
Analog: a synthetic chemical or pharmaceutical drug that behaves very much like a normal chemical in the body.
Anandron: trade or brand name for nilutamide.
Anatomy: the study of the structure of the body and the relationship between its parts.
Androgen: a hormone which is responsible for male characteristics and the development and function of male sexual organs (e.g. testosterone).
Anemia: a reduction below normal in the oxygen-carrying capacity of the blood.
Anesthesia: the loss of feeling or sensation caused by a drug or gas. General anesthesia causes loss of consciousness with local anesthesia numbs only a certain area.
Aneuploid: having an abnormal number of sets of chromosomes; e.g., tetraploid means having two paired sets of chromosomes, which is twice as many as normal (see also “Diploid”).
Anterior: The front; e.g., the anterior of the prostate is the part of the prostate that faces forward.
Anti-androgen: a compound (usually a synthetic pharmaceutical drug) which blocks or otherwise interferes with the normal action of androgens. Usually used in combination with orchiectomy or LHRH analogs.
Antibiotic: a pharmaceutical that can kill certain types of bacteria.
Antibody: protein produced by the immune system as a defense against an invading or “foreign” material or substance (for example, when you get a cold, your body produces antibodies to the cold virus).
Anticholinergic: an agent that blocks nerves that are not under conscious control.
Anti-coagulant: a pharmaceutical drug that helps to stop the blood from clotting.
Antigen: “foreign” material introduced into the body (a virus or bacterium, for example) or other material which the immune system considers to be “foreign” because it is not part of the body’s normal biology (e.g., prostate cancer cells).
Anus: the opening of the rectum.
Apex: the tip or bottom of the prostate, i.e., the part of the prostate farthest away from the bladder
Artificial sphincter: prosthesis or artificial device sometimes used to treat incontinence after prostate surgery.
Aspiration: the use of suction to remove fluid or tissue, usually through a fine needle (e.g., aspiration biopsy).
Asymptomatic: having no recognizable symptoms of a particular disorder.
B
Base: the base of the prostate is the wide part at the top of the prostate closest to the bladder.
Benign: relatively harmless; not cancerous; not malignant; not potentially fatal.
Benign prostatic hyperplasia: see “BPH”.
Bias: a point of view preventing impartial judgment on issues. In clinical trials “blinding” and “randomization” serve to minimize bias.
Bicalutamide: a non-steroidal anti-androgen available in the U.S. and some European countries for the treatment of advanced prostate cancer.
Bilateral: both sides; e.g., a bilateral orchiectomy is an operation in which both testicles are removed and a bilateral adrenalectomy involves removal of both adrenal glands.
Biofeedback: a procedure that uses electrodes to help people gain awareness and control of their pelvic muscles.
Biophosphanate: medication used to increase bone density to avoid fracture and decrease the likelihood of bone pain.
Biopsy: sampling of tissue from a particular part of the body (e.g., the prostate) in order to check for abnormalities such as cancer; in the case of prostate cancer, biopsies are usually carried out under ultrasound guidance using a specially designed device known as a prostate biopsy gun.
Bladder: the hollow sac-like organ in which urine is collected and stored in the body.
Blind: a randomized clinical trial is considered blind when the participants do not know whether they are in the group being given the experimental treatment (experimental group) or the group that is receiving the best available standard treatment (control group).
Bone scan: a sensitive technique which uses radiolabelled agents to identify abnormal or cancerous growths within or attached to bone; in the case of prostate cancer, a bone scan is used to identify bony metastases which are definitive for cancer which has escaped from the prostate.
Bowel preparation: the cleaning of the bowels or intestines which is normal prior to abdominal surgery such as radical prostatectomy.
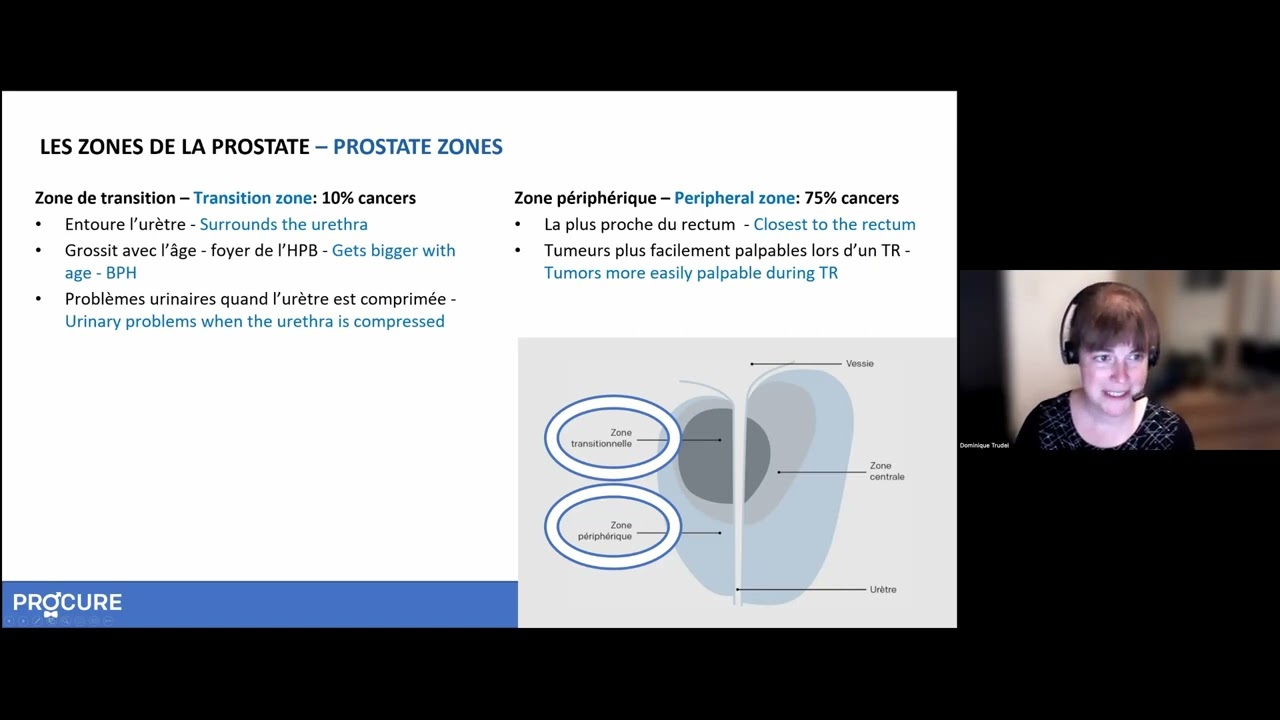
BPH: benign prostatic hyperplasia or enlargement of the prostate occurs in most men age they age; it can cause difficulties for many men (such as the frequent need to urinate at night), which can become severe for some individuals.
Brachytherapy: the implantation of radioactive seeds or pellets which emit low energy radiation in order to kill surrounding tissue (e.g., the prostate, including prostate cancer cells).
Bulbous urethra: enlarged section of the urethra downstream from where the urethra passes through the prostate. Seminal fluid collects in the bulbous urethra before ejaculation.
Buserelin acetate: a luteinizing hormone releasing hormone analog used in the palliative hormonal treatment of advanced prostate cancer and sometimes in the adjuvant and neoadjuvant hormonal treatment of earlier stages of prostate cancer.
C
CAB: complete androgen blockade (see “Maximal androgen deprivation”).
Cancer: the growth of abnormal cells in the body in an uncontrolled manner.
Capsule: the fibrous tissue which acts as an outer lining of the prostate.
Carcinoma: another word meaning cancer.
Casodex: brand name or trade name of bicalutamide.
Castration: the use of surgical or medical techniques to lower the level of testosterone in the male to zero or near zero.
Catheter: a hollow (usually plastic) tube that can be used to drain fluids from or inject fluids into the body…
Chemoprevention: the use of a pharmaceutical drug or other substance to prevent the development of cancer.
Chemotherapy: the use of pharmaceutical drugs to kill cancer cells…
Chromosome: threadlike structure in every cell that consists of genes composed of DNA…
CHT: combined hormone therapy or treatment (see “Maximal androgen deprivation”).
Clinical trial: a carefully planned experiment to evaluate a treatment or a medication…
Collagen: colloidal chemical substance made of proteins…
Complication: an unexpected or unwanted effect of a treatment…
Conformational therapy: the use of careful planning and delivery techniques designed to focus radiation…
Congestion: situation characterized by buildup of fluid in some area of the body…
Continence: ability to retain urine.
Contracture: scarring that can occur at the bladder neck after a radical prostatectomy…
Control group: the group in the clinical trial that receives the best available standard treatment.
Cooperative groups: networks of organizations and researchers…
Corpus cavernosum: two chambers running the length of a man’s penis…
Corpus spongiosum: a spongy chamber in a man’s penis that contains the urethra…
Cryoablation: see “Cryosurgery”.
Cryosurgery: the use of liquid nitrogen to freeze a particular organ…
Cryotherapy: see “Cryosurgery”.
CT scan: computerized tomography…
Cystoscope: an instrument used by physicians to look inside the bladder…
Cystoscopy: the use of a cystoscope to look inside the bladder and the urethra.
D
Debulking: reduction of the volume of cancer by one of several techniques…
DES: see “Diethylstilbestrol.”
DHT: see “Dihydrotestosterone.”
Diagnosis: the evaluation of signs, symptoms, and selected test results…
Diethylstilbestrol: a female hormone commonly used in the 1960’s and 1970’s…
Differentiation: the process of changing from an original unspecialized form…
Digital rectal examination: the use by a physician of a lubricated and gloved finger…
Dihydrotestosterone: the male hormone active in the prostate…
Diploid: having one complete set of normally paired chromosomes…
DNA: deoxyribonucleic acid…
Double-blinded study: a form of clinical trial…
Doubling time: the time that it takes a particular focus of cancer to double…
Downsizing: the use of hormonal or other forms of management…
Downstaging: the use of hormonal or other forms of management…
DRE: see “Digital rectal examination”.
Drip collector: collecting device, either internal or external…
Dysplasia: see “Prostatic intraepithelial neoplasia”.
E
Ejaculate: the sperm-containing fluid (semen)…
Ejaculation: sudden discharge of semen…
Eligard: brand or trade name of leuprolide acetate…
Emcyt: brand or trade name of estramustine phosphate…
Enzyme: a protein produced in cells…
Epididymis: two comma-shaped tubes inside the scrotum…
Erectile dysfunction: the inability to obtain or maintain an erection…
Erection: a mechanism that allows for rigidity…
Estramustine phosphate: a chemotherapeutic agent used…
Estrogen: one of the most important female hormones…
Eulexin: the brand or trade name of flutamide…
Experimental: an unproven (or even untested) technique…
External beam: a form of radiation therapy…
F
Fibrosis: the formation of a scar.
Fistula: an abnormal passage or communication…
5-alph reductase: an enzyme found in the prostate…
Flutamide: an anti-androgen used in the palliative hormonal treatment…
Foley catheter: type of catheter named for its inventor…
Free PSA: PSA that is not bound to proteins.
Frequency: the need to urinate often.
G
Gastrointestinal: related to the digestive system…
Gene: one of many discrete units of hereditary information…
Gene therapy: a new type of treatment in which defective genes are replaced…
Genital system: the biological system which, in males…
Genito-urinary system: the combined genital and urinary systems…
Gland: a structure or organ that produces a substance…
Glaucoma: a group of eye diseases characterized by an increase in intraocular pressure…
Gleason: name of physician who developed the Gleason grading system…
Goserelin acetate: a luteinizing hormone releasing hormone analog…
Grade: a means of describing the potential degree of severity of a cancer…
Gynecomastia: enlargement or tenderness of the male breasts…
H
Hematospermia: the occurrence of blood in the semen.
Hematuria: the occurrence of blood in the urine.
Heredity: the historical distribution of biological characteristics through a group of related individuals via their DNA.
Hereditary: inherited from one’s parents and earlier generations.
Histology: the study of the appearance and behaviour of tissue, usually carried out under a microscope by a pathologist (who is a physician) or a histologist (who is not necessarily a physician).
Homogeneous: uniform, of the same kind.
Hormone: a biologically active chemical responsible for the development of secondary sexual characteristics.
Hormone therapy: the use of hormones, hormone analogs, and certain surgical techniques to treat disease (in this case advanced prostate cancer) either on their own or in combination with other hormones or in combination with other methods of treatment.
Hot flash: the sudden sensation of warmth in the face, neck and upper body, a side effect of many forms of hormone therapy.
Hyperplasia: enlargement of an organ or tissue because of an increase in the number of cells in that organ or tissue; see also “BPH.”
I
Imaging: a technique or method allowing a physician to see something that would not normally be visible.
Immune system: the biological system that protects a person or animal from the effects of foreign materials such as bacteria viruses, cancer cells, and other things that might make that person or animal sick.
Implant: a device inserted into the body in order to replace or substitute for an ability that has been lost; for example, a penile implant is a device that can be surgically inserted into the penis to provide rigidity for intercourse.
Impotence: the inability to have or to maintain an erection.
Incidental: insignificant or irrelevant; for example, incidental prostate cancer (also known as latent prostate cancer) is a form of prostate cancer that is of no clinical significance to the patient in whom it is discovered.
Incontinence: leaking of or inability to control any substance, but commonly the leaking of or inability to control urine (properly called urinary incontinence).
Indication: a reason for doing something or taking some action; also used to mean the approved clinical application of a pharmaceutical drug.
Infertility: in a man with prostate problems, the inability to father a child due to prostate infection or retrograde ejaculation.
Inflammation: any form of swelling or pain or irritation.
Informed consent: in the case of a clinical trial, it means that you know what the trial is about, you understand why it is being conducted and why you have been invited to take part, and you appreciate exactly how you will be involved.
Interstitial: within a particular organ; for example, interstitial prostate radiation therapy is radiation therapy applied within the prostate using implanted radioactive pellets or seeds (see also “Brachytherapy”).
Interstitial cystitis: a chronic inflammatory condition of the bladder.
Intravenous: into a vein.
Intravenous pyelogram: a procedure that introduces a radioactive substance into the urinary tract in order to allow the physician a superior image of the tract by taking an X-ray.
Invasive: requiring an incision or the insertion of an instrument or substance into the body.
IVP: see “Intravenous pyelogram”.
K
Kegel exercises: a set of exercises designed to improve the strength of the muscles of the pelvic floor, in order to augment urinary control and prevent leakage.
Kidney: one of a pair of organs whose primary function is to filter the fluids passing through the body.
L
Laparoscopic lymph node dissection: test procedure using a device called a laparoscope that involves the removal of tissue through small incisions for later examination of possibly cancerous lymph nodes in the vicinity of the prostate.
Laparoscopy: a technique allowing the physician to observe internal organs directly through a piece of optical equipment inserted directly into the body through a small surgical incision.
Latent: insignificant or irrelevant; for example, latent prostate cancer (also known as incidental prostate cancer) is a form of prostate cancer of no clinical significance to the patient in whom it is discovered.
Leuprolide acetate: a luteinizing hormone-releasing hormone analog used in the palliative hormonal treatment of advanced prostate cancer and sometimes in the adjuvant and neoadjuvant hormonal treatment of earlier stages of prostate cancer.
LH-RH: see “Luteinizing hormone releasing hormone”.
LH-RH analog: a man-made hormone that is chemically similar to LH-RH.
Libido: interest in sexual activity.
Lobe: one of the two sides of an organ that clearly has two sides (e.g. the prostate or the brain).
Localized: restricted to a well-defined area.
Lupron: brand or trade name of leuprolide acetate in the U.S. and Canada.
Luteinizing hormone-releasing hormone: a hormone responsible for stimulating the production of testosterone in the body.
Lycopene: the major red pigment in some fruit.
Lymph: the clear fluid in which all of the cells in the body are constantly bathed, also known as the lymphatic fluid.
Lymphadenectomy: a surgical procedure in which the lymph nodes are dissected.
Lymph node: any of the many small structures that filter lymph and produce lymphocytes. Lymph nodes are concentrated in several areas of the body, such as the armpit, groin, and neck.
Lymphocyte: a white blood cell that normally makes up 25 percent of the total white blood cell count but increases in the presence of infection. Lymphocytes aid in the protection of the body against illness.
M
MAB: maximal androgen blockade (see “Maximal androgen deprivation”).
MAD: see “Maximal androgen deprivation.”
Magnetic resonance imaging: a technique allowing sophisticated vertical, cross-sectional, and even three-dimensional images of organs inside the body based on the electromagnetic properties of different atomic particles as opposed to X-rays.
Male sling: surgery whereby a sling is used to compress the urethra to stop any leakage of urine during such activities as coughing, sneezing or exercising.
Malignancy: a growth or tumour composed of cancerous cells.
Malignant: cancerous.
Margin: normally used to mean the “surgical margin,” which is the outer edge of the tissue removed during surgery; if the surgical margin shows no sign of cancer (“negative margins”), then the prognosis is good.
Maximal androgen deprivation: the combined use of two forms of hormonal treatment to block the effects of testosterone and other androgens produced by the adrenal glands (also known by many other names and abbreviations).
Medical oncologist: a doctor who specializes in chemotherapy, which involves the use of drugs to treat cancer. He or she also has a wide experience in relieving physical symptoms such as pain and emotional, psychological or spiritual concerns.
Metastasis: a secondary tumour formed as a result of a cancer cell or cells from the primary tumour site (e.g. the prostate) travelling through the body to a new site and then growing there.
Metastatic: having the characteristics of a secondary tumour.
Metastron: the brand or trade name of strontium-89 in the U.S.
Misstaging: the assignment of an incorrect clinical stage at initial diagnosis because of the difficulty of assessing the available information with accuracy.
Mixed incontinence: exhibiting symptoms of both stress and urge incontinence.
Monoclonal: formed from a single group of identical cells.
MRI: see “Magnetic resonance imaging.”
Multi-centre clinical trial: also called multi-site clinical trial; trial that takes place at many different sites at the same time.
Myasthenia gravis: disease whose characteristic feature is easy fatigue of certain voluntary muscle groups on repeated use.
N
Negative: the term used to describe a test result that does not show the presence of the substance or material for which the test was carried out; for example, a negative bone scan would show no sign of bone metastases.
Neoadjuvant: added before; for example, neoadjuvant hormone therapy is therapy given prior to another form of treatment such as a radical prostatectomy.
Neoplasia: the growth of cells under conditions that would tend to prevent the development of normal tissue (e.g. a cancer).
<>Neoplasm: any abnormal growth in the body. May be benign or malignant.
Nerve sparing: term used to describe a type of prostatectomy in which the surgeon saves the nerves that affect sexual and related functions.
Neurogenic bladder: a dysfunction due to a malfunction of the nerves responsible for the control of bladder function.
Nilutamide: an anti-androgen, still experimental in the U.S., but available in Canada and some other countries.
Nitrates: medications used to treat chest pain.
Nocturia: the need to urinate frequently at night.
Non-invasive: not requiring any incision nor the insertion of an instrument or substance into the body.
O
Oncologist: a physician who specializes in the treatment of various types of cancer.
Orchiectomy: the surgical removal of the testicles.
Organ: a group of tissues that work in concert to carry out a specific set of functions (e.g. the heart or the lungs or the prostate).
Osteoporosis: reduction of bone mass leading to fractures after minimal trauma.
Overactive bladder: a condition characterized by involuntary bladder muscle contractions that cannot be suppressed.
Overflow incontinence: the loss of small amounts of urine from a bladder that is always full. Also called paradoxical incontinence.
Overstaging: the assignment of an overly high clinical stage at initial diagnosis because of the difficulty of assessing the available information with accuracy (e.g. stage T3b as opposed to stage T2b).
P
Palliative: designed to relieve a particular problem or problems without necessarily solving them; for example, palliative therapy is given in order to relieve symptoms and improve quality of life but not to cure the patient.
Palpable: capable of being felt during a physical examination by an experienced physician; in the case of prostate cancer, this normally refers to some form of abnormality of the prostate that can be felt during a digital rectal examination.
PAP: see “Prostatic acid phosphatase.”
Pathologist: a physician who specializes in the examination of tissues and blood samples to help decide what diseases are present and how they should be treated.
Pelvic floor muscles exercises: see “Kegel exercises.”
Pelvic node dissection: removal of the lymph nodes in the pelvis.
Pelvis: that part of the skeleton that joins the lower limbs of the body.
Penile: of the penis.
Penile implant: prosthesis or artificial device used to treat impotence. When surgically inserted into the penis, it provides sufficient rigidity for vaginal penetration and sustained sexual intercourse.
Penis: the male organ used in urination and intercourse.
Perineal: of the perineum.
Perineal prostatectomy: surgical removal of the prostate through an incision between the scrotum and anus.
Perineum: the area of the body between the scrotum and the rectum.
Peripheral: outside the central region.
Peyronie’s disease: a disease of unknown cause in which plaques form around the corpus cavernosum of the penis, causing deviation and painful erection.
PIN: see “Prostatic intraepithelial neoplasia.”
Pituitary gland: gland at the base of the brain that produces hormones stimulating release of other hormones, including testosterone.
Placebo: a safe but inactive (fake) pill, liquid or powder that is used as a basis for comparison with pharmaceuticals in research studies.
Ploidy: a term used to describe the number of sets of chromosomes in a cell; see also “Diploid and aneuploid.”
Positive: the term used to describe a test result that shows the presence of the substance or material for which the test was carried out; for example, a positive bone scan would show signs of bone metastases.
Posterior: the rear; for example, the posterior of the prostate is the part of the prostate that faces a man’s back.
Priapism: a persistent abnormal erection of the penis accompanied by pain and tenderness that requires medical attention.
Prognosis: the patient’s potential clinical outlook based on the status and probable course of his disease.
Progression: continuing growth or regrowth of the cancer.
Prostascint scan: a scan that uses low-level radioactive material to find cancer that has spread beyond the prostate.
Prostate: the spherical gland, about the size of a walnut, surrounding the urethra and immediately below the bladder in males. Secretes part of the seminal fluid and controls urinary flow.
Prostate-specific antigen (PSA): a protein made by the prostate gland and detected in the blood. Its presence increases in response to the presence of foreign materials such as prostate cancer cells; it is used to detect potential problems in the prostate gland.
Prostate-specific antigen density (PSAD): metric determined by dividing the PSA number by the prostate volume (its size as measured by transrectal ultrasound).
Prostatectomy: a surgical removal of the prostate gland; see also “Radical prostatectomy.”
Prostatic acid phosphatase (PAP): an enzyme test now used only rarely to decide whether prostate cancer has escaped from the prostate.
Prostatic intraepithelial neoplasia: also called prostatic intraductal neoplasia. a pathologically identifiable condition believed to be a possible precursor of prostate cancer; also known more simply as dysplasia by many physicians.
Prostatitis: infection or inflammation of the prostate gland.
Prostatosis: chronic pain of the prostate.
Prosthesis: a man-made device used to replace a normal body part or function.
Protocol: a precise set of methods by which a research study is to be carried out.
PSA: see “Prostate-specific antigen.”
PSAD: see “Prostate-specific antigen density.”
Q
Quality of life: an evaluation of health status relative to the patient’s age, expectations, and physical and mental capabilities.
R
Radiation oncologist: a physician who has received special training regarding the treatment of cancers with different types of radiation.
Radiation therapy: (also known as radiotherapy) the use of X-rays in an attempt to destroy malignant tissues.
Radical prostatectomy: the surgical removal of the prostate and surrounding tissue and structures with the intent to cure the problem believed to be caused by or within the prostate.
Radioisotope: a type of atom (or a chemical made with a type of atom) that emits radioactivity.
Radiologist: physician who specializes in radiology, administering and interpreting X-ray, ultrasound and other imaging studies.
Radiology: a branch of medicine concerned with X-rays, ultrasound and other imaging techniques.
Randomization: the process of assigning patients by a method of chance to different forms of treatment (either the experimental group or the control group) in a research study. A way to prevent bias in research.
Rectum: the final part of the intestines ending at the anus.
Recurrence: the reappearance of disease.
Refractory: resistant to therapy.
Regression: reduction in the size of a single tumour or reduction in the number or size of several tumours.
Remission: the real or apparent disappearance of some or all of the signs and symptoms of cancer.
Resection: surgical removal of tissue.
Resectoscope: instrument inserted through the urethra and used by a urologist to cut out tissue (usually from the prostate) while seeing precisely where he is cutting.
Resistance: (in a medical sense) a patient’s ability to fight off a disease as a result of the effectiveness of his (or her) immune system.
Retention: difficulty in initiation of urination or the ability to completely empty the bladder.
Retropubic: behind or posterior to the pubic arch.
Retropubic prostatectomy: prostatectomy in which a surgical incision is made through the abdomen at a point above where the penis enters the body, cutting through the bladder to reach the prostate.
Reverse transcriptase polymerase chain reaction (RTPCR): a technique that allows a physician to search for tiny quantities of a protein, such as PSA, in the blood or other body fluids and tissues.
Risk: the chance or probability that a particular event will or will not happen.
RTPCR: see “Reverse transcriptase polymerase chain reaction.”
S
Salvage: a procedure intended to “rescue” a patient following the failure of a prior treatment, for example a salvage prostatectomy would be the surgical removal of the prostate after the failure of prior radiation therapy or cryosurgery.
Screening: the search for disease, such as cancer, in people without symptoms.
Scrotum: the pouch of skin containing a man’s testicles.
Secondary tumour: a tumour that spreads (metastasis) from the site where it started.
Seeds: radioactive pellets implanted in the prostate to destroy cancerous growth.
Selenium: a relatively rare non-metallic element that is found in small quantities in food and that may have some effect in prevention of cancer.
Semen: the whitish, opaque fluid emitted by a male at ejaculation.
Seminal: related to the semen.
Seminal vesicles: glands at the base of the bladder and connected to the prostate that add nutrients to the semen.
Serum: the clear liquid portion of the blood (excluding the blood cells).
Sextant: having six parts; thus, a sextant biopsy is a biopsy requiring six samples.
Side effect: a reaction to a medication or treatment (most commonly used to mean an unnecessary or undesirable effect).
Sign: physical changes that can be observed as a consequence of an illness or disease.
Single-centre clinical trial: also called single-site clinical trial; a trial that takes place at only one site and is initiated by one researcher.
Social worker: an individual who specializes in drawing on community resources to benefit people facing a major life crisis. He or she will help you make adjustments and adapt to changing social and economic environments.
Sphincter: the ring of muscles located around the urethra that regulates the passage of urine.
Stage: a term used to define the size and physical extent of a cancer.
Staging: the process of assigning a stage to a particular cancer in a specific patient in light of all the available information.
Stent: a tube used by a surgeon to drain fluids.
Stress incontinence: leakage of urine as a result of physical exertion such as coughing, sneezing, lifting an object and/or exercising.
Stricture: scarring as a result of a procedure or an injury that constricts the flow of a fluid; for example, a urethral stricture would restrict the flow of urine through the urethra.
Strontium-89: an injectable radioactive product used to relieve bone pain in some patients with prostate cancer that no longer responds to hormones or appropriate forms of chemotherapy.
Subcapsular: under the capsule; for example, a subcapsular orchiectomy is a form of castration in which the contents of each testicle is removed but the testicular capsules are then closed and remain in the scrotum.
Suprapubic: above the pubic arch.
Suprapubic prostatectomy: prostatectomy in which a surgical incision is made through the abdomen at a point above where the penis enters the body, bypassing the bladder as the cut is extended to the prostate.
Suprefact: brand or trade name of buserelin acetate in the U.S. and Canada.
Suture: surgical stitching used in the closure of a cut or incision.
Symptom: a feeling, sensation, or experience associated with or resulting from a physical or mental disorder and noticeable by the patient.
Systemic: throughout the whole body.
T
TAB: total androgen blockade; see “Maximal androgen deprivation.”
Testis: one of two male reproductive glands located inside the scrotum which are the primary source of the male hormone testosterone; plural testes.
Testicle: see “Testis.”
Testosterone: the male hormone or androgen that makes up about 90 percent of the androgens in a man’s body; it is needed to complete male sexual function and fertility.
Total androgen blockade (TAB): see “Maximal androgen deprivation.”
Transition: change; for example, the transition zone of the prostate is the area of the prostate closest to the urethra and has features which distinguish it from the much larger peripheral zone.
Transperineal: through the perineum.
Transrectal: through the rectum.
Transrectal ultrasound: a method of imaging the prostate by inserting an ultrasound probe into the rectum; commonly used to visualize prostate biopsy procedures.
Transurethral: through the urethra.
Transurethral hyperthermia (TH): new treatment for benign prostate enlargement; heat generated by a microwave transmitter alleviates urinary obstruction.
Transurethral incision of the prostate (TUIP): new treatment for benign prostate enlargement; a series of small cuts is made inside the urethra to alleviate urinary obstruction.
Transurethral resection of the prostate (TURP): a surgical procedure in which part of the prostate gland surrounding the urethra is removed using a resectoscope.
Transurethral ultrasound-guided laser prostatectomy: new prostatectomy technique used with benign prostate enlargement; a laser beam guided by an ultrasound image removes excess prostate tissue that interferes with normal urination.
TRUS: see “Transrectal ultrasound.”
TUIP: see “Transurethral incision of the prostate.”
Tumour: an abnormal tissue growth that can be either benign or malignant.
TURP: see “Transurethral resection of the prostate.”
U
Ultrasound: use of ultra high-frequency sound waves to image internal organs and structures (e.g. a baby in the womb).
Understaging: the assignment of an overly low clinical stage at initial diagnosis because of the difficulty of assessing the available information with accuracy (e.g. stage T2b as opposed to stage T3b).
Unit: a surgical term for a pint (usually of blood).
Ureter: an anatomical tube that drains urine from one of the two kidneys to the bladder.
Urethra: the tube that drains urine from the bladder through the prostate and out through the penis.
Urge incontinence: the leakage of urine that occurs when the bladder has involuntary contractions. There is a strong feeling of having to urinate right away and not making it on time to the toilet.
Urgency: the need to urinate right away.
Urinary system: the group of organs and their interconnections that permit excess, filtered fluids to exit the body; including (in the male) the kidneys, the ureters, the bladder, the urethra and the penis.
Urinary tract infection (UTI): an infection identifiable by the presence of bacteria in the urine; may be associated with fever, or a burning pain on urination.
Urologist: a doctor trained first as a surgeon who specializes in disorders of the genito-urinary system.
UTI: see “Urinary tract infection.”
V
Vas deferens: tube through which sperm travel from the testes to the prostate prior to ejaculation.
Vasectomy: operation to make a man sterile by cutting the vas deferens, thus preventing passage of sperm from the testes to the prostate.
Vesicle: a small saclike part (e.g. seminal vesicle) containing fluid.
W
Watchful waiting: follow-up of patients with prostate cancer until symptoms appear or the cancer spreads, at which time hormone therapy is usually given to reduce symptoms and disease progression.
Z
Zoladex: brand or trade name of goserelin acetate in the U.S. and Canada.
Zone: part or area of an organ.
Additional Information - Glossary and publications
Urologist’s advice: Treatments and information on prostate cancer
Learn more about the role of the urologist and the importance for a patient to gather adequate information after receiving a prostate cancer diagnosis.
How I coped with prostate cancer
A man with prostate cancer shares the challenges of his cancer experience.
Genetics and prostate cancer
Do you have a family history of cancer? Your doctor might recommend genetic screening.
Symptoms, risk and screening
Are you over 50 or experiencing urinary problems? Discover why early screening for prostate diseases is important.
Prostate cancer prognosis and survival
After a prostate cancer diagnosis, questions about survival, cure rates, and quality of life can arise.

Prostate cancer: Tests, imaging and biomarkers
This webinar covers various tests and exams for diagnosing and monitoring prostate cancer.
Biopsy: Understanding your report
This webinar clarifies biopsy reports, pathologists’ roles, and how results confirm or rule out prostate cancer.

Your prognosis and survival
After receiving a diagnosis of prostate cancer, you will undoubtedly have questions about your prognosis and survival and will want to know the chances of success with your treatment.
What is a genetic mutation?
Do you have a significant family history of cancer? Is there a link between prostate cancer and a genetic mutation?

Finding the right words
Prostate cancer often overwhelms patients. Finding the right words is crucial to comfort and support them.

Link between prostate cancer and obesity
If you are obese or overweight, it is more likely that prostate cancer will be diagnosed at a more advanced stage…

Prostate cancer: Is it a disease of the elderly?
It depends on the definition of old. Is being 50 years old really considered “old”?

What women should know about prostate cancer
As a woman, you might think that prostate cancer is not your concern because you don’t have a prostate. However, prostate cancer is the most common cancer in men.

I was told no to the PSA test
The PSA test should generally be offered to any man aged 50 and over with a life expectancy of at least ten years. So why this refusal?

Me a guinea pig?
Did you know that participating in a clinical trial advances medical science and improves the lot of patients for future generations?

Your role as a patient
Have you been diagnosed with prostate cancer? Your role as a patient is essential throughout your journey.
Sources and references
Last medical and editorial review: April 2024. See our web page validation committee and our collaborators by clicking here.


