Brachytherapy
Brachytherapy
The word brachy- originates from the Greek word brachys, meaning “short”. Therefore, “brachytherapy” means treatment with radiation therapy at a short distance, as opposed to “teletherapy”, also known as external beam radiotherapy. Brachytherapy is a type of radiation therapy involving the insertion of radioactive materials directly in the specific tissue being treated, in this case, the cancerous prostate. Radiation destroys cancer cells over time.

The administration of brachytherapy is done in two ways:
Low-dose rate or permanent brachytherapy: in this case, the radioactivity dose is very low but permanent. Permanent implants, such as radioactive seeds, are not removed. They release their radiation dose over a few weeks or months.
High-dose rate or temporary brachytherapy: in this case, a very strong radioactive substance is temporarily inserted directly into the prostate using catheters connected to a radiation source. Temporary implants are removed once the desired radiation dose has been delivered.
Low-dose rate brachytherapy is primarily used for low-risk or intermediate-risk prostate cancer corresponding to specific medical criteria. External beam radiotherapy may be combined with high-dose rate brachytherapy for high-risk prostate cancer that is likely to progress.
The most commonly used radioactive materials in brachytherapy for prostate cancer treatment are iodine, iridium, and cesium.
The time it takes for the radioactivity of a substance to decrease by half is called the half-life. Different radioactive materials have different half-lives. This information helps the radiotherapy team choose the type of material to use and plan the treatment protocol. It also determines how long safety measures need to be followed after treatment.
Is it for you
Low-dose rate or permanent brachytherapy
Low-dose rate brachytherapy (LDR), often referred to by its English acronym LDR (Low Dose Rate), delivers very low radiation doses. They are emitted from small sources containing radioactive iodine, called “iodine 125.”
These sources resemble grains of rice. They remain in the prostate forever. However, their radioactivity decreases over time. After 6 months, 95% of the radioactivity is gone. The presence of sources does not cause any long-term problems.
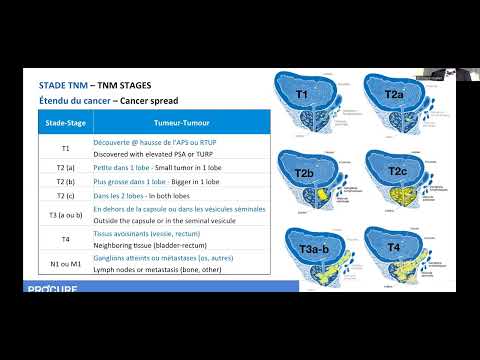
This treatment may be offered to you if you have been diagnosed with localized cancer, at a relatively early stage (T1, T2a), slow-growing, hence at low risk of progression (Gleason 6 or less), and with a low PSA level (below 10 ng/ml). It may be an option for intermediate-risk cancers (Gleason 7), but patients are highly selected based on specific criteria.
High-dose rate or temporary brachytherapy
High-dose rate brachytherapy (HDR), often referred to by its English acronym HDR (High Dose Rate), delivers high radiation doses. They are emitted from small sources containing radioactive iridium, called “iridium 192.”
This type of brachytherapy can be administered as a complement to external beam radiation therapy or as a single treatment for prostate cancer (high-dose monotherapy), with or without hormone therapy
Used as a complement: Increasingly, high-dose rate brachytherapy is considered a means of dose intensification in any patient receiving external beam radiation therapy for prostate cancer treatment. This helps reduce the number of conventional radiotherapy treatments. This approach is particularly useful for intermediate and high-risk patients.
Used as monotherapy: Although not recommended as the sole treatment for men with high-risk prostate cancer, it is increasingly used as monotherapy for low-risk or intermediate-risk cancers.
This treatment may be offered to you regardless of the risk of progression of your cancer (low, intermediate, or high).
Additional considerations
Brachytherapy may not be recommended:
- To men who have significant symptoms of prostatism related to urinary obstruction or who have undergone transurethral resection of the prostate.
- To men whose prostate cancer has metastasized, based on bone scans or CT scans of the abdomen and pelvis.
- To men who have undergone pelvic radiotherapy, have hip problems, or are targeted by any other contraindication.
Remarks: Due to the expensive expertise and technology involved, this treatment is not available in all hospitals.
Factors justifying this choice
For many men with localized prostate cancer, brachytherapy offers an effective treatment without the risks and recovery times associated with surgery.
Advantages of brachytherapy
- Quick recovery, so most men can return to their normal activities shortly after treatment.
- No hospitalization required: it’s a one-day procedure.
- Radiation does not pass through the skin or other healthy organs to reach cancer cells. Brachytherapy therefore causes less damage to neighboring organs.
- Less demanding treatment than traditional radiotherapy and less taxing than radical prostatectomy.
- No recovery period or operative stress, as with radical prostatectomy.
Disadvantages of brachytherapy
- You will generally need to have general anesthesia, which can have side effects.
- The exact nature and extent of your tumor cannot be known as precisely as after surgery.
- Failures can only rarely be treated surgically (the exception). Radiotherapy may have damaged the prostate and surrounding tissues, making prostate removal more difficult and increasing the risk of side effects.
- You will experience a significant decrease in ejaculate and loss of fertility if you want children.
- You will need to avoid sitting very close to pregnant women or children for more than a few minutes each day, for the first three months after treatment.
Risks and complications of brachytherapy
Some adverse effects may occur immediately after the procedure or a few weeks later. Generally, they are temporary, may last a few months, and gradually disappear within the year following the end of treatment.
Short-Medium term
The side effects of brachytherapy are similar to those of external beam radiotherapy but differ slightly. As the prostate has been punctured multiple times, this treatment causes it to swell. This can cause urinary problems, with symptoms such as:
- Frequent urination, especially at night.
- Urgent need to urinate (urgency).
- Difficulty urinating with a weaker stream.
- Burning sensation when urinating.
- Sometimes even complete urinary blockage (acute urinary retention).
Pain in the perineum, presence of blood in the urine or semen, and transient erection problems may occur following treatment.
Irritation of the intestines and rectal disorders, such as inflammation of the rectum, are uncommon. However, diarrhea, anal irritation, or rectal bleeding may occur in the months following treatment, although very rare.
Long term
Late effects may occur months or even years after this treatment. Side effects vary and may include:
- Erectile dysfunction.
- The risks of urinary incontinence or symptoms of chronic urinary obstruction are rare (in both cases, less than 5%).
These effects depend greatly on your condition before the intervention. A person who already had good erections OR few urinary problems is less at risk of consequences.
It is important to report any side effects to your doctor.
Whether short-medium or long term, most can be relieved by taking medication or other interventions/methods.


Your doctor has suggested brachytherapy to treat your prostate cancer? This section describes this treatment and precautions to ensure the best outcome. Click here for a better understanding of medical terms related to your male reproductive system.
Brachytherapy (LDR) procedure details
Duration of procedure
The procedure takes one to two hours, but including preparation, calculations, and recovery, it may take up to eight hours in some cases.
Insertion of a urinary catheter
A spinal (local) anesthesia or, less commonly, a general anesthesia is administered. A urinary catheter is inserted during the procedure and removed at the end. In extremely rare cases, the catheter remains in place for some time to facilitate urine passage.
The procedure
Using transrectal ultrasound, a specialist precisely inserts the seeds into the prostate at predetermined locations. An experienced radiation oncologist implants between 80 and 100 radioactive seeds into the prostate.
Seed localization
The radioactive seeds implanted in the prostate gradually kill cancer cells over hours and days. A special CT scan will be performed three to six weeks after the procedure to locate the final position of the seeds and calculate doses.
Your PSA level
With brachytherapy, it’s not expected for the PSA level to drop to 0 ng/mL as it’s practically impossible to destroy 100% of prostate cells. Typically, the PSA level decreases and stabilizes afterward.
Brachytherapy (HDR) procedure details
Duration of procedure
The procedure takes two to three hours in the treatment room, and the patient can leave in the evening. In rare cases, the doctor may decide to keep the patient longer.
Insertion of a urinary catheter
A general anesthesia is administered. A urinary catheter is inserted during the procedure and removed at the end. In extremely rare cases, the catheter remains in place for some time to facilitate urine passage.
The procedure
The doctor inserts small empty plastic tubes (12 to 18 catheters or even more) into the skin, between the scrotum and the anus. These tubes are then inserted deeper into the body, up to the prostate using a probe. The tubes are connected to a treatment device. This device delivers a radioactive source (Iridium 192) through the tubes. The treatment lasts 20 to 30 minutes.
Your PSA level
With brachytherapy as a complement to external beam radiotherapy, it’s not expected for the PSA level to drop to 0 ng/mL as it’s practically impossible to destroy 100% of prostate cells. Typically, the PSA level decreases and stabilizes afterward.
In monotherapy
For high-dose monotherapy, the treatment is one to two doses in a day surgery setting. The patient is hospitalized during the treatment. No radioactivity is emitted when the catheters are not connected to the device, and the patient can rest in the general urology department between interventions without needing to be isolated.
Preparation before brachytherapy
Good preparation can make the recovery period after brachytherapy less challenging than expected. Your preparation will play a crucial role in a faster and less stressful recovery. By reading the following on this page, you will know what to expect and how to cope.
Questions to my doctor
We invite you to consult our page Questions to ask to your doctor and your healthcare team regarding tests and diagnostic exams for prostate cancer. Asking questions will open up communication, provide information tailored to your situation, and reduce the stress associated with understanding the diagnosis of prostate cancer.
Before the start of treatment
Shortly before beginning your treatment, you will meet with your medical team to prepare for and commence your treatment.
A few weeks before treatment
You may receive a call to schedule an appointment at a pre-admission clinic. There, you will undergo various tests to complete your health assessment.
The day before treatment
You must not eat or drink anything after midnight. If you need to take medication, you can have a small amount of water. You will need to perform a rectal enema, as instructed.
On the day of treatment
Inform the doctor of all medications you usually take. Bring them in their original containers. You will be given an antibiotic by infusion before the procedure.
Bring to the hospital a not-too-tight pair of underwear that you feel comfortable in, and an absorbent pad. You will be more comfortable when you return home.
The process of these interventions
The process of permanent brachytherapy (with seeds) and temporary brachytherapy differs depending on the treatment. To learn more about the process of these interventions, click here .
Convalescence following brachytherapy
High dose-rate brachytherapy: Your return home and instructions to follow are similar to those described for external radiotherapy treatment. Low dose-rate brachytherapy requires only a short recovery period.
To learn more about discomforts after your treatment, safety measures, and resumption of sexual activities, click here.
Medical follow-up
Medical certificate
If you need a medical certificate, remember to request it directly from your radiation oncologist.
Success rate
As with radical prostatectomy, it is impossible to establish a general success rate with brachytherapy.
- This varies depending on each case because the diagnosed grade of the tumor, its stage of spread, and the PSA level before treatment must be taken into account.
- The lower these data are, the better the chances that the patient will be definitively cured.
PSA test
Rectal examination and prostate-specific antigen (PSA) test, performed regularly – every three to six months – allow your radiation oncologist to monitor your condition. The PSA test is the best predictor of prostate cancer recurrence.
Your PSA level
With brachytherapy, it is not expected that the PSA level will drop to 0 ng/mL since normal prostate cells still remain. Usually, the PSA level drops to a plateau and remains there. Your level should start to decrease in the months following the start of treatment. It may even continue to decrease one year after treatment.
At each follow-up appointment, your radiation oncologist will evaluate three parameters:
- if the PSA level increases
- how long after treatment it occurred
- and how long it takes for this level to double (this is its velocity)
Recurrence
If the PSA level starts to rise, the doctor will monitor how long it takes to double. The shorter these periods, the greater the risk of recurrence, and the more aggressive the recurrence will be. For example, a PSA level that starts to rise eight months after the end of treatment and doubles in six months is much more concerning than a PSA level that starts to climb three years after this intervention and takes one year to double.
If necessary, hormone therapy may be prescribed. Otherwise, discuss with your radiation oncologist the options for salvage treatments after brachytherapy.
Remission
You will be followed up for at least five years after your radiotherapy. After seven to ten years without recurrence, the risks of the cancer returning are then low.
Side effects
The side effects of brachytherapy depend on the following factors:
- the type of implants (temporary or permanent)
- the volume of the treated area
- the dose of radiation that may have reached neighboring organs, usually very low
- the total dose received
Some side effects occur immediately after the intervention or a few weeks later. Generally, they are temporary. Others appear well after the intervention and can last a long time. The most common problems associated with brachytherapy are urinary, gastrointestinal, and erectile function issues.
Intestinal and urinary function
Sometimes intestinal and urinary functions take longer to return to normal at the end of treatment.
- Some medications – such as suppositories or cortisone enemas that help reduce rectal inflammation – and muscle relaxants that can sometimes provide relief – may be prescribed.
- Request an appointment with a nutritionist or dietitian for your intestinal problems.
- Discuss your urinary problems with your doctor. Often, they can be easily corrected with medication or intervention.
To learn more about urinary and intestinal disorders, see our section on side effects.
Erectile function
The percentage risk of erectile dysfunction can vary from patient to patient. However, unlike other side effects, erectile dysfunction gradually appears several months or even years after treatment, but does not affect enjoyment.
- Since cell death is progressive, you will retain your erectile capacity for several years, but it will decrease over time.
- Your erectile capacity depends on your sexual function before treatment, your age, and your overall health.
To learn more about erectile dysfunction, see our section on sexual disorders.
Additional Information - Treatment options
Medical monitoring and care management
Are you undergoing treatment for prostate cancer? Various approaches can help monitor it.
Urinary and sexual problems after treatment
Prostate cancer treatments can lead to side effects, such as erectile dysfunction and urinary incontinence, which vary in intensity and duration.
Everything to know about radical surgery
Considering radical surgery for your cancer treatment? Watch this webinar to learn about the procedure, its benefits, drawbacks, and suitability for you.
Surveillance, surgery or radiation therapy?
Diagnosed with prostate cancer? Several treatment options are available based on the stage, age, and your health.
Active surveillance as a treatment option?
Did you know that in many cases it is not necessary to treat prostate cancer?

I was told about leaks, not incontinence
It is not uncommon to have calls from patients asking us why they suffer from incontinence following radical surgery to treat their prostate cancer.

I have 4 treatment options; confused, you say?
If being diagnosed with prostate cancer is a massive blow for men, the treatment options can quickly become a headache…

Active surveillance in 5 points
As surprising as it may seem, your doctor may prefer to wait before starting treatment.
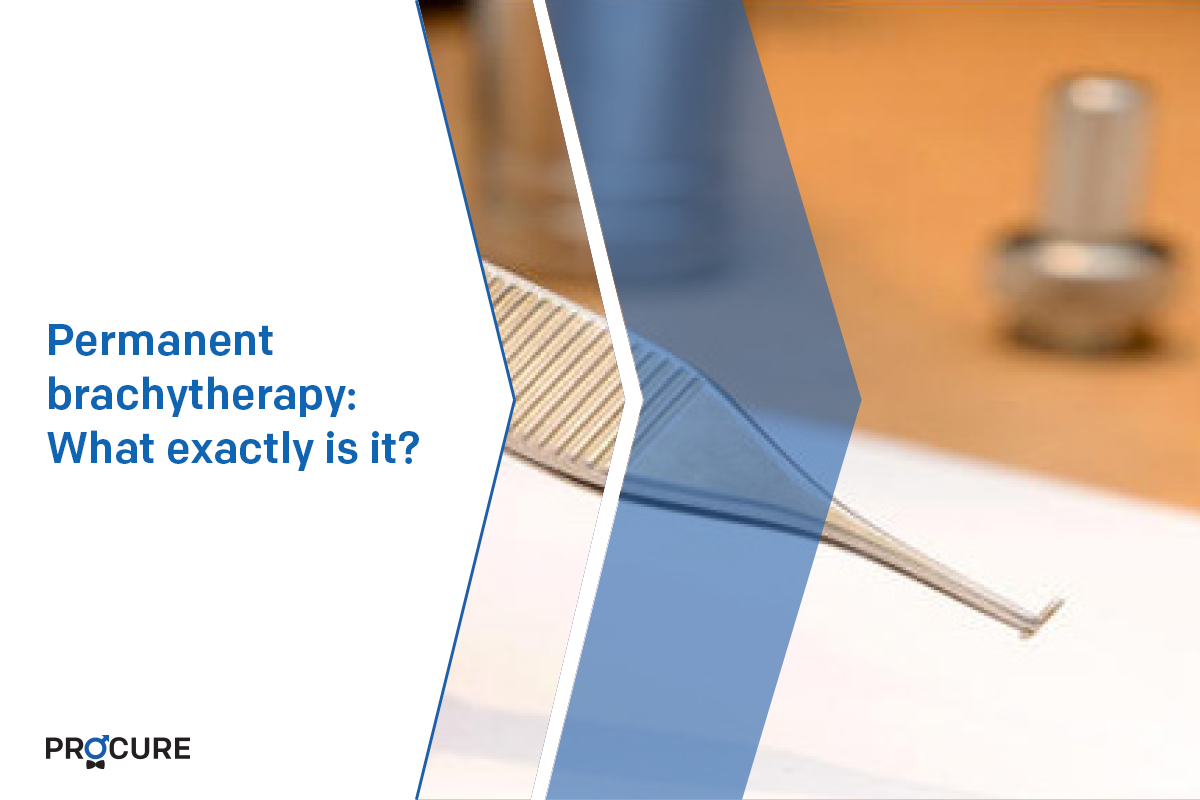
Permanent brachytherapy: What exactly is it?
Permanent brachytherapy often called low dose rate brachytherapy, administers very small doses of radiation. They are emitted from small sources containing radioactive iodine, called “iodine 125”. These sources look like grains of rice. They stay in your prostate forever. However, their radioactivity decreases over time. After 6 months, 95% of the radioactivity has disappeared. The presence of these sources does not cause any long […]

Radical surgery: 5 points to remember
If you’ve been diagnosed with prostate cancer, your doctor will consider many factors before recommending the best treatment. For many of you, this may mean completely removing the prostate, which is radical surgery. Here are 5 points to remember if you are considering this option. Radical surgery: Is it for you? Radical surgery is the most common […]
Conventional or robotic surgery?
Here is a typical case of concern from a patient who has opted for radical surgery as a treatment for his cancer and who asks the famous question: Which surgery is better? Conventional or robotic surgery? Before answering it, let’s take a look at the context in which the question was asked of our nurses […]

Choice between radical surgery or radiotherapy?
Unless you are not a candidate for either option, there are generally no strict rules for deciding whether radical surgery or radiotherapy is preferable as a treatment. If your cancer is really confined to your prostate, it can be cured with surgery or radiation therapy. However, to benefit from a cure, your life expectancy must be […]

Recovery timeline after surgery
Recovery timeline after surgery, that is after radical prostate surgery, varies from person to person depending on how their body heals naturally and the severity of the disease before surgery. Here are some tips to help you with your recovery timeline. Plan your return home After surgery, you will not necessarily have the energy to […]

What is successful active surveillance
Is it possible to achieve successful active surveillance? Of course. Does this mean your cancer will never progress? Not at all. But in 65-70% of cases, cancer does not progress because the patient was a good candidate for this type of treatment option. Having prostate cancer does not necessarily mean that you will be treated. […]
Sources and references
Last medical and editorial review: April 2024. See our web page validation committee and our collaborators by clicking here.



